Podcast 168: Gait Speed, hip extension, and A New Dawn
/Podcast 168: Gait Speed, hip extension, and A New Dawn
Join us each month on the Masterclass in Gait, link below
https://www.patreon.com/thegaitguys
Join at the $40 monthly level and get the masterclass each month, bonus material and the detailed monthly content we only share on Patreon.
The Masterclass is a formal LIVE presentation of slides, videos, demos, deep dives on topics you will not hear anywhere but here ! We hit the gait, biomechanics, neurology and orthopedics of all of the gait topics we present. This is not for the weak and timid, this is the deep dive you have been waiting for. Join us while we turn our normal 50 minute presentations into 3.5 hours on a regular basis ! The 40$ Patreon level will give you the Masterclass and also get you the $20, $10, and 5$ Patreon level content. What a deal ! It will not be here forever so lock in now !
Or, you can get less for your money (why would you do that?) and just buy our Monthly $40 Masterclass at our VIMEO on demand page: https://vimeo.com/ondemand/thegaitmasterclass
Links to find the podcast:
Look for us on Apple Podcasts, Google Play, Podbean, PlayerFM, RADIO and more.
Just Google "the gait guys podcast".
https://traffic.libsyn.com/secure/thegaitguys/pod_169_March_12_-_32821_10.19_AM.mp3
https://thegaitguys.libsyn.com/gait-speed-hip-extension-and-a-new-dawn
https://directory.libsyn.com/episode/index/id/18496787
_______________________________________________________________________________
Our Websites:
www.thegaitguys.com
Find Exclusive content at: https://www.patreon.com/thegaitguys
doctorallen.co
summitchiroandrehab.com
shawnallen.net
Our website is all you need to remember. Everything you want, need and wish for is right there on the site.
Interested in our stuff ? Want to buy some of our lectures or our National Shoe Fit program? Click here (thegaitguys.com or thegaitguys.tumblr.com) and you will come to our websites. In the tabs, you will find tabs for STORE, SEMINARS, BOOK etc. We also lecture every 3rd Wednesday of the month on onlineCE.com. We have an extensive catalogued library of our courses there, you can take them any time for a nominal fee (~$20).
Our podcast is on iTunes and just about every other podcast harbor site, just google "the gait guys podcast", you will find us.
Where to find us, the podcast Links:
Apple podcasts:
https://itunes.apple.com/us/podcast/the-gait-guys-podcast/id559864138?mt=2
Google Play:
https://play.google.com/music/m/Icdfyphojzy3drj2tsxaxuadiue?t=The_Gait_Guys_Podcast
Dual decline in gait speed and cognition is associated with future dementia: evidence for a phenotype
Age Ageing. 2020 Oct 23;49(6):995-1002. doi: 10.1093/ageing/afaa106.
Manuel Montero-Odasso et. al
Walking in humans: how much brain function is needed?
Kressig RW.
Age Ageing. 2020 Oct 23;49(6):930-931
Correlations Between Hip Extension Range of Motion, Hip Extension Asymmetry, and Compensatory Lumbar Movement in Patients with Nonspecific Chronic Low Back Pain
Med Sci Monit. 2020 Sep 24;26:e925080. doi: 10.12659/MSM.925080
Won-Deuk Kim 1 , DooChul Shin 2
Prolonged sitting and physical inactivity are associated with limited hip extension: A cross-sectional study
Musculoskelet Sci Pract. 2021 Feb;51:102282. doi: 10.1016/j.msksp.2020.102282. Epub 2020 Oct 28. Abderrahmane Boukabache 1 , Stephen J Preece 1 , Nathan Brookes 2
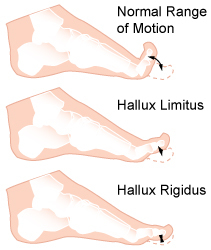
Independent muscle of extensor hallucis capsularis: a cadaveric case report
Surg Radiol Anat. 2020 Oct 13. doi: 10.1007/s00276-020-02592-7. Online ahead of print.
Jeong-Hyun Park , Yu-Jin Choi, Kwang-Rak Park , Digud Kim , Hyung-Wook Kwon , Mijeong Lee, Jaeho Cho
Sensorimotor and gait training improves proprioception, nerve function, and muscular activation in patients with diabetic peripheral neuropathy: a randomized control trial
J Musculoskelet Neuronal Interact. 2020 Jun 1;20(2):234-248.
Irshad Ahmad , Shalini Verma , Majumi M Noohu , Mohd Yakub Shareef , M Ejaz Hussain