If you are a sprinter, how you load the forefoot bipod might be a variable for speed or injury. Tendons can change their cross sectional area, if you load them.
/Of course this article is not exclusive for sprinters, it pertains to any running sport, even endurance.
Maximum isometric force had increased by 49% and tendon CSA by 17% !
Tendons can change their cross sectional area, if you load them.
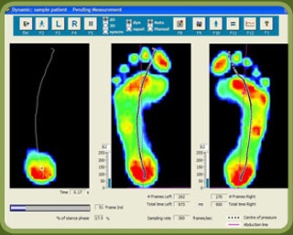
Here I show lateral forefoot loading in a heel raise, and a medial forefoot loading in heel raise. This has to be part of the discovery process outlined below. Forefoot types will play into the loading choice, and unequal strength of the medial or lateral calf compartment will also play into the loading choice made. Where do you need to put your strength ? And is the forefoot competent to take that loading challenge ? Meaning, do they have a forefoot valgus? A forefoot supinatus ? These things matter. If you are a sprinter, how you load the forefoot bipod might be a variable of foot type, asymmetrical posterior compartment strength, or foot strike pattern in the frontal plane (search our blog for cross over gait and glute medius targeting strategies for step width) ,or a combination of several or all of the above. These things matter, and why and where you put your strength matters, if you are even aware of where and how you are putting the loads, and why of course. Of course, then there are people like the recent Outside online article that says how you foot strike doesn’t matter, but it does matter. But of course, if you do not know the things we have just mentioned, it is easy to write such an article.
Isometrics are useful, they have their place. In a recent podcast we discussed the place and time to use isometrics, isotonics, eccentrics and concentrics.
One of the goals in a tendinopathy is to restore the tendon stiffness. Isometrics are a safe way to load the muscle tendon complex without engaging a movement that might have to go through a painful arc of movement. With isometrics here is neurologic overspill into the painful arc without having to actually go there.
The key seems to be load. More load seems to get most people further along. Remember, the tendon is often problematic because it is inflammed and cannot provide a stiffness across its expanse. Heavy isometric loading seems to be a huge key for most cases. But, we have to say it here, not everyone fits this mold. Some tendons, in some people, will respond better to eccentrics, and strangely enough, some cases like stretching (perhaps because this is a subset of an eccentric it seems or because there is a range of motion issue in the joint that is a subset of the problem). Now the literature suggests that stretching is foolish, but each case is unique all in its own way, and finding what works for a client is their medicine, regardless of what the literature and research says.
Finding the right load for a given tendon and a right frequency of loading and duraction of loading is also case by case specific. Part of finding the right loading position is a discovery process as well, as noted in the photos above. Finding the fascicles you want to load, and the ones you do not want to load (painful) can be a challenging discovery process for you and your client. Finding the right slice of the pie to load, and the ones not to load takes experimentation. When it is the achilles complex, finding the safe However, if one is looking for a rough template to build from, brief, often, heavy painfree loads is a good template recipe to start with.
Here, in this Geremia et al article, "ultrasound was used to determine Achilles tendon cross-sectional area (CSA), length and elongation as a function of plantar flexion torque during voluntary plantar flexion."
They discovered that, "At the end of the training program, maximum isometric force had increased by 49% and tendon CSA by 17%, but tendon length, maximal tendon elongation and maximal strain were unchanged. Hence, tendon stiffness had increased by 82%, and so had Young’s modulus, by 86%.
Effects of high loading by eccentric triceps surae training on Achilles tendon properties in humans. Jeam Marcel Geremia, Bruno Manfredini Baroni, Maarten Frank Bobbert, Rodrigo Rico Bini, Fabio Juner Lanferdini, Marco Aurélio Vaz
European Journal of Applied Physiology
August 2018, Volume 118, Issue 8, pp 1725–1736