Podcast 169: Foot muscles, core strength and more
/Podcast 167: Foot muscles, core strength and more
Join us each month on the Masterclass in Gait, link below
https://www.patreon.com/thegaitguys
Join at the $40 monthly level and get the masterclass each month, bonus material and the detailed monthly content we only share on Patreon.
The Masterclass is a formal LIVE presentation of slides, videos, demos, deep dives on topics you will not hear anywhere but here ! We hit the gait, biomechanics, neurology and orthopedics of all of the gait topics we present. This is not for the weak and timid, this is the deep dive you have been waiting for. Join us while we turn our normal 50 minute presentations into 3.5 hours on a regular basis ! The 40$ Patreon level will give you the Masterclass and also get you the $20, $10, and 5$ Patreon level content. What a deal ! It will not be here forever so lock in now !
Or, you can get less for your money (why would you do that?) and just buy our Monthly $40 Masterclass at our VIMEO on demand page: https://vimeo.com/ondemand/thegaitmasterclass
Links to find the podcast:
Look for us on Apple Podcasts, Google Play, Podbean, PlayerFM, RADIO and more.
Just Google "the gait guys podcast".
https://traffic.libsyn.com/secure/thegaitguys/pod_169_March_12_-_32821_10.19_AM.mp3
https://thegaitguys.libsyn.com/gait-speed-hip-extension-and-a-new-dawn
https://directory.libsyn.com/episode/index/id/18496787
_______________________________________________________________________________
Our Websites:
www.thegaitguys.com
Find Exclusive content at: https://www.patreon.com/thegaitguys
doctorallen.co
summitchiroandrehab.com
shawnallen.net
Our website is all you need to remember. Everything you want, need and wish for is right there on the site.
Interested in our stuff ? Want to buy some of our lectures or our National Shoe Fit program? Click here (thegaitguys.com or thegaitguys.tumblr.com) and you will come to our websites. In the tabs, you will find tabs for STORE, SEMINARS, BOOK etc. We also lecture every 3rd Wednesday of the month on onlineCE.com. We have an extensive catalogued library of our courses there, you can take them any time for a nominal fee (~$20).
Our podcast is on iTunes and just about every other podcast harbor site, just google "the gait guys podcast", you will find us.
Where to find us, the podcast Links:
Apple podcasts:
https://itunes.apple.com/us/podcast/the-gait-guys-podcast/id559864138?mt=2
Google Play:
https://play.google.com/music/m/Icdfyphojzy3drj2tsxaxuadiue?t=The_Gait_Guys_Podcast
Podcast links:
https://traffic.libsyn.com/secure/thegaitguys/168_feb_12.2021_-_4321.mp3
https://thegaitguys.libsyn.com/pod-foot-muscles-core-strength-and-more
https://directory.libsyn.com/episode/index/id/18589871
@IreneSDavis
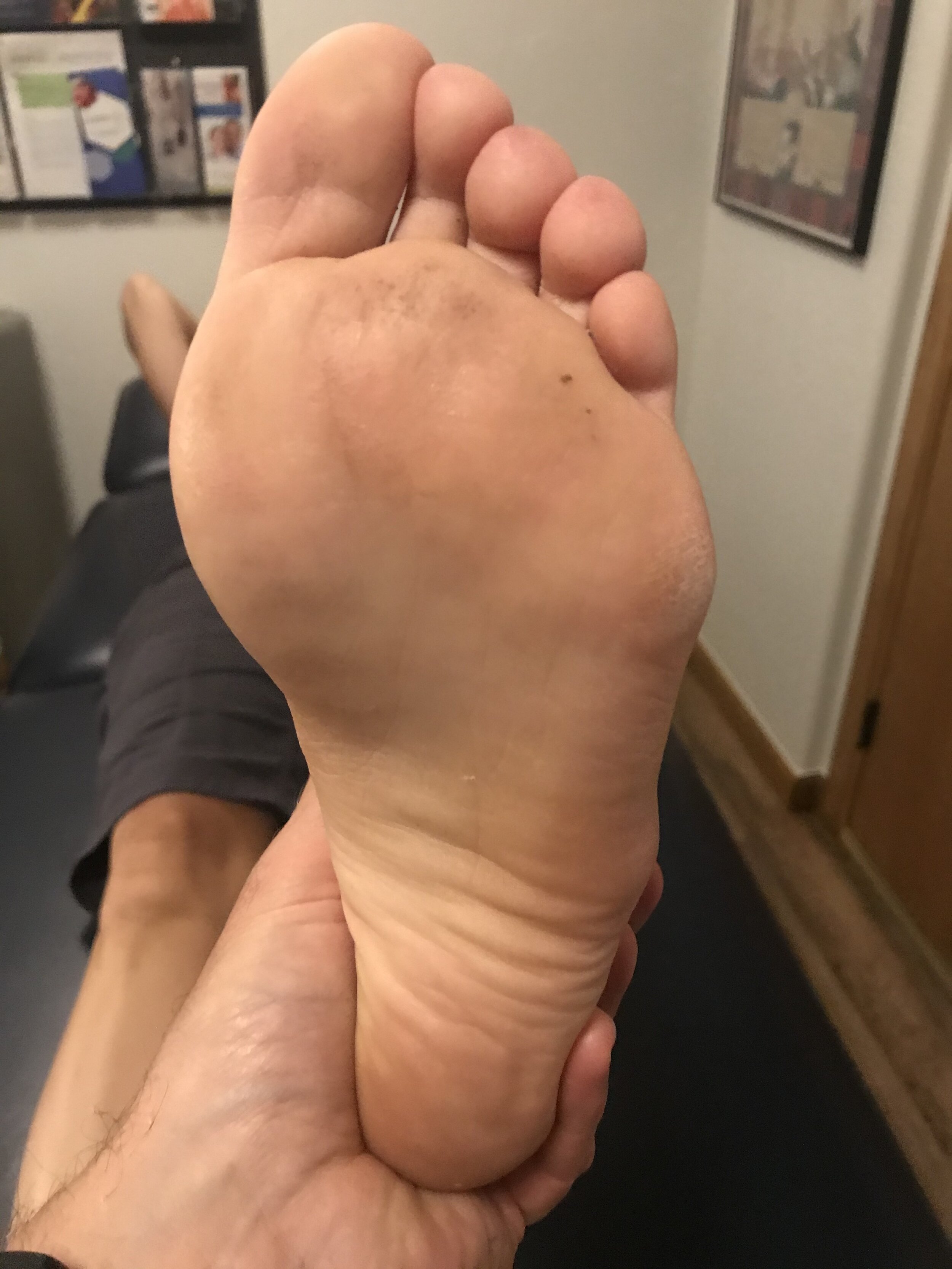
Numerous studies demo foot muscle hypertrophy when removing support of the arch. While it seems intuitive, this is the first published study to demo that adding support results in foot muscle atrophy after only 12 weeks of orthotic use! Nice work!! #strengtheningoverbracing
https://journals.sagepub.com/doi/abs/10.1177/0363546520969205
Foot Core Training to Prevent Running-Related Injuries: A Survival Analysis of a Single-Blind, Randomized Controlled Trial
Ulisses T. Taddei, PhD, PT, Alessandra B. Matias, MSc, PT, Marcos Duarte, PhD,
https://twitter.com/IreneSDavis/status/1306033740020408320/photo/1
https://pubmed.ncbi.nlm.nih.gov/32521283/
2020 Aug;78:105063. clinbiomech.2020.105063.
The effect of a 12-week custom foot orthotic intervention on muscle size and muscle activity of the intrinsic foot muscle of young adults during gait termination
Katrina Protopapas 1 , Stephen D Perry 2
_______
hip abduction
https://www.tandfonline.com/doi/abs/10.1080/02640414.2020.1820183?journalCode=rjsp2
Inter-limb strength asymmetry in adolescent distance runners: Test-retest reliability and relationships with performance and running economy
Rich Blagrove
Summary: Key finding: Larger hip abduction asymmetry associated with worse running economy in female runners (r = 0.85).
____________
Developing neurplasticity
SPlit treadmills , limping,
https://pubmed.ncbi.nlm.nih.gov/23312637/
_____________
quick talk on bone density
https://twitter.com/rwilly2003/status/1303526386846461952?s=1
https://journals.physiology.org/doi/abs/10.1152/jappl.1992.73.3.1165
Relationship among running mileage, bone density, and serum testosterone in male runners: J. D. MacDougal