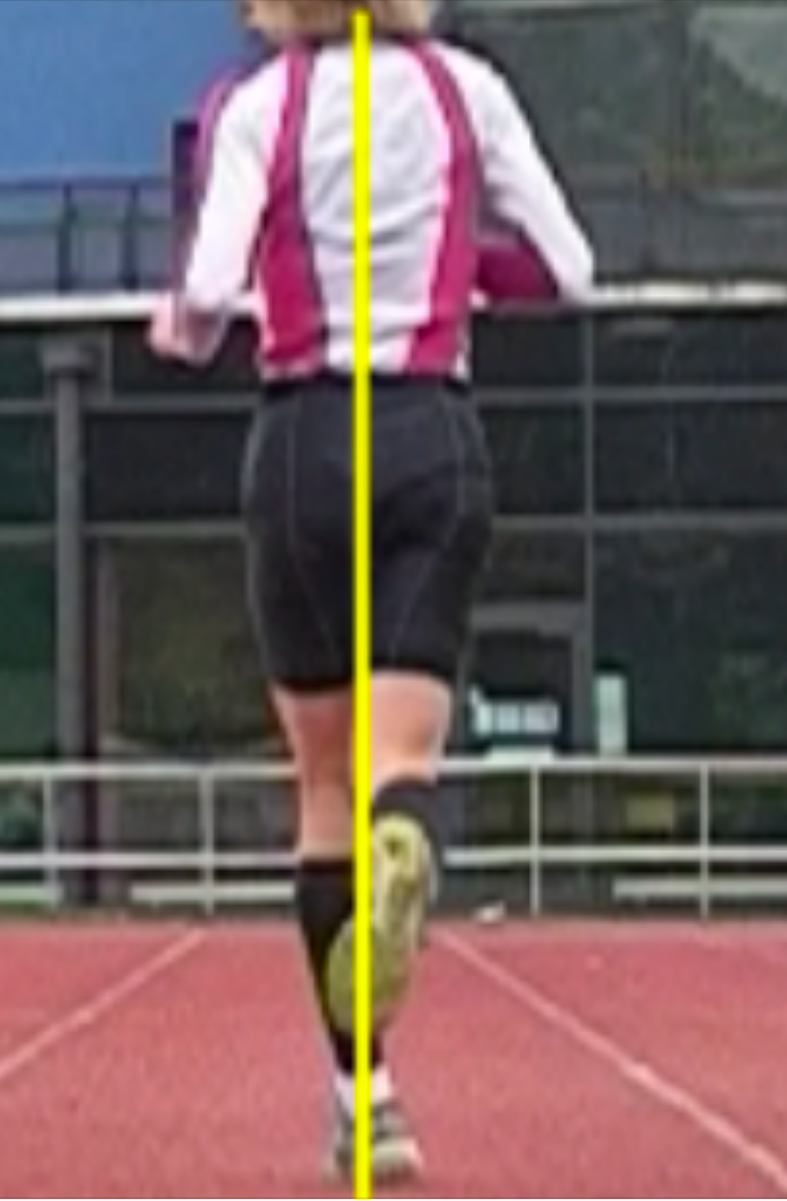
We get “help me” emails from all over the world on a regular basis. Recently we received this photo from a runner in Oxford, UK, often we cannot help, but when there is a story to tell that everyone can learn from, we offer what we can. This runner was frustrated, explaining a “dodgy foot”. We like the word.
dodg·y däjē/
-dishonest or unreliable; potentially dangerous; of low quality.
We can likely guarantee you that the solution here to this runner’s form issue is not wholly at the foot which appears “in toed” and slanted and appears ready to kick the back of the right heel, not to mention the knees that are about to brush together. Thus, merely working on their foot strike would be so remedial and corrupt that it would a crime.
Ivo and I do not take on cases via the internet because we cannot give all the information because we cannot examine the client, many do offer such services but people are not being given the whole story and we pledged long ago not to be part of the problem. Anyone who recommends exercises from things they see on a video gait analysis are basically doing the same disservice in our opinion. But sometimes, as in this case, their inquiry offers a opportunity for dialogue. This is one of those cases. I will not be presenting a solution, because I do not have the examination information I need, but I will propose a thought process that further investigation may afford progress towards some answers.
This appears like a non-pathologic cross over gait in my mind until proven otherwise, there may be other sources, causes and components, but when it quacks like a duck you’d be silly not to check for webbed feet. There are many component parts that leave someone with a cross over type gait (ie a narrow based gait, that if taken further, might as well result in running on a line). This runner even confirmed upon questioning that the left foot scuffs the inside of the right ankle/shin often, both sides scuff in fact but more left shoe on right shin. No Einsteinian epiphany there.
This means a narrow swing through (adducting) left limb.
This might mean stance and swing phase gluteus medius communication problems.
This might mean swing leg foot targeting problems.
This often suggests right, but sometimes both right and left, frontal plane pelvis sway problems which means pelvis control is challenged which means core lumbar stability control is challenged.
This means adaptive arm swing changes from the clean norm. Arm swing to a large degree is driven by the lower limb motor patterns, despite what some people will propose (dive into our archives to find some of those research articles).
This does NOT mean this runner has pain, or pain yet, or maybe never will have pain but there are many determinants of that which I will discuss below.
But, make no mistake, this is flawed gait mechanics, but that does not translate to injury, speed, outcome or pain. But when they come with those complaints attached, one would be foolish not to at least consider these biomechanics as a source.
The left swing leg is clearly targeting a more medial placement, meaning limb adduction (active or passive or both is to be determined) and this is a product of the cross over gait (unfamiliar with the cross over gait ? SEARCH our blog for the term, you will need a few hours of free time to get through it all). Some would call the cross over gait a lazy gait, but I would rather term it an efficient gait taken too far that it has now become a liability, a liability in which they can no longer stabilize frontal plane sway/drift. A wider gait on the other hand, as in most sprinters, is less efficient but may procure more power and the wider base is more stable affording less frontal plane drift. Just go walk around your home and move from a very narrow line walking gait to a wide gait and you will feel a more powerful engagement of the glutes. Mind you, this is not a fix for cross over gaits, gosh, if it was only that simple !
This runner might investigate whether there is right frontal plane drift, and if it is in fact occurring, find the source of the drift. It can come from many places on either limb. (This client says they are scuffing both inside ankles, which is not atypical and so we likely have drift on both right and left). We have discussed many of them here in various places on the blog over the years. Now as for “Why” the foot looks in toed, well that can also come from many places. Quite simply the adducted limb once it leaves toe off (a toe off that is most often a "low gear toe off", meaning not a medial/hallux toe off), can look like this. But, perhaps it is also a product of insufficient external rotation maintenance occurred during that left stance phase, affording more internal rotation which is being unchecked and observed here during early swing. Remember though, if this is in fact a cross over gait result, in this gait the limb approaches the ground unstacked (foot is too far inside a left hip joint plumb line) the foot will greet the ground at a far lateral strike and in supination. Pronation will thus be magnified and accelerated, if there is enough time before toe off. However, and you can try this on your own by walking around your home, put yourself in terminal stance at toe off. Make sure you have the foot inverted so you are toeing off the lateral toes (low gear toe off). Does this foot not look like the one in the photo ? Yes it does, now just lift the foot off the ground and you have reproduced this photo. And when combined with a right pelvis drift, the foot will sneak further medially appearing postured behind the right foot.
Keep this in mind as well, final pronation and efficient hallux (big toe) toe off does often not occur in someone who strikes the ground on a far lateral foot. I am sure this runner will now be aware of how poorly they toe off of the big toe, the hallux. They will tend to progress towards low gear toe off, off the lesser toes. This leaves the foot inverted and this is what you are seeing in her the photo above. That is a foot that is inverted and supinated and it carried through all the way through toe off and into early swing. It is a frequently component of the cross over gait, look for it, you will find it, often.
Final thoughts, certainly this can be an isolated left swing phase gluteus medius weakness enabling an adducted swing limb thus procuring a faulty medial foot placement, but it is still part of the cross over phenomenon. Most things when it comes to a linked human frame do not work in isolation. But i will leave you with a complicating factor and hopefully you will realize that gait analysis truly does require a physical exam, and without it you could be missing the big picture problem. What if she has a notable fixed anatomic internal tibia torsion on that left side. Yup, it could all be that simple, and that is not something you can fix, you learn to manage that one as a runner.
* Side bar rant: Look at any google search of runners photos and you will see this type of swing limb foot posturing often, far too often. That does not mean it is normal ! That means, that many people do this, but it cannot mean that it is optimal mechanics. And yes, you can take the stance that “I do it as well and i have no injuries or problems so what is the big deal?”. Our response is often “you do have an issue, it may be anatomic or functional, but you do have an asymmetrical gait and you think it is not a problem, YET”. And maybe you will run till you are 6 feet under and not have a problem because you have accommodated over many years and you are a great compensator, yes, some people get lucky. Some people also do not run enough miles that these issues express themselves clinically so lets be fair. But some of these people are reality deniers and spend their life buying the newest brace or gadget, trying a different shoe insert, orthotic or new shoe of the month and shop over and over again for another video gait analysis expert who can actually fix their pain or problem. And then there are those who have a 45 minute home exercise program that they need to do to keep their problems at bay, managing, not fixing anything. Or, they spend an hour a week on the web reading article after article on what are the top 4 exercises for iliotibial band syndrome for example. They shop for the newest Graston practitioner, the newest kinesio taping pattern, Voodoo bands, breathing patterns, compression socks etc. And sometimes they are the ones that say they still don't have a problem.You get the drift. Gosh darn it, find someone who knows what the hell they are doing and can help you fix the issues that are causing the problem. And yes, some of the above accoutrements may be assistive in that journey.
I have dealt with this unique toe off issue very frequently. Once you see something enough times, you learn all of the variations and subtle nuances that a problem can take on. But, trying to fit everyone into a similar solution model is where the novice coach, trainer or clinician will get into trouble. Trust us, it all starts with an examination, a true clinical physical examination. If one leaves the investigatory process to a series of screens or functional movement patterns, “activation” attempts, digital gait analysis or strength tests one is juggling chainsaws and the outcome you want is often not likely to occur. There is nothing wrong with making these components part of the investigation process, but on their own, they are not enough to get the honest answer many times. Of course, Ivo and i were not able to jump the pond and examine this runner with our own eyes and hands so today’s dialogue was merely to offer this runner some food for thought to open their mind to our thought process, in the hopes that they can find someone to help them solve the underlying problem and not merely make the gait look cleaner. Making someone’s walking or running gait look cleaner is not hard, but making it subconsciously competent and clean (without thought or effort) requires a fix to the underlying problem. We can ALMOST guarantee you that the solution here to this runner’s form issue is not wholly at the foot that looks in toed and slanted. Merely working on their foot strike would be so remedial and corrupt that it would a crime.
Dr. Shawn Allen, one of the gait guys
#gait, #gaitproblems, #crossovergait, #gaitanalysis, #gluteweakness, #toeoff