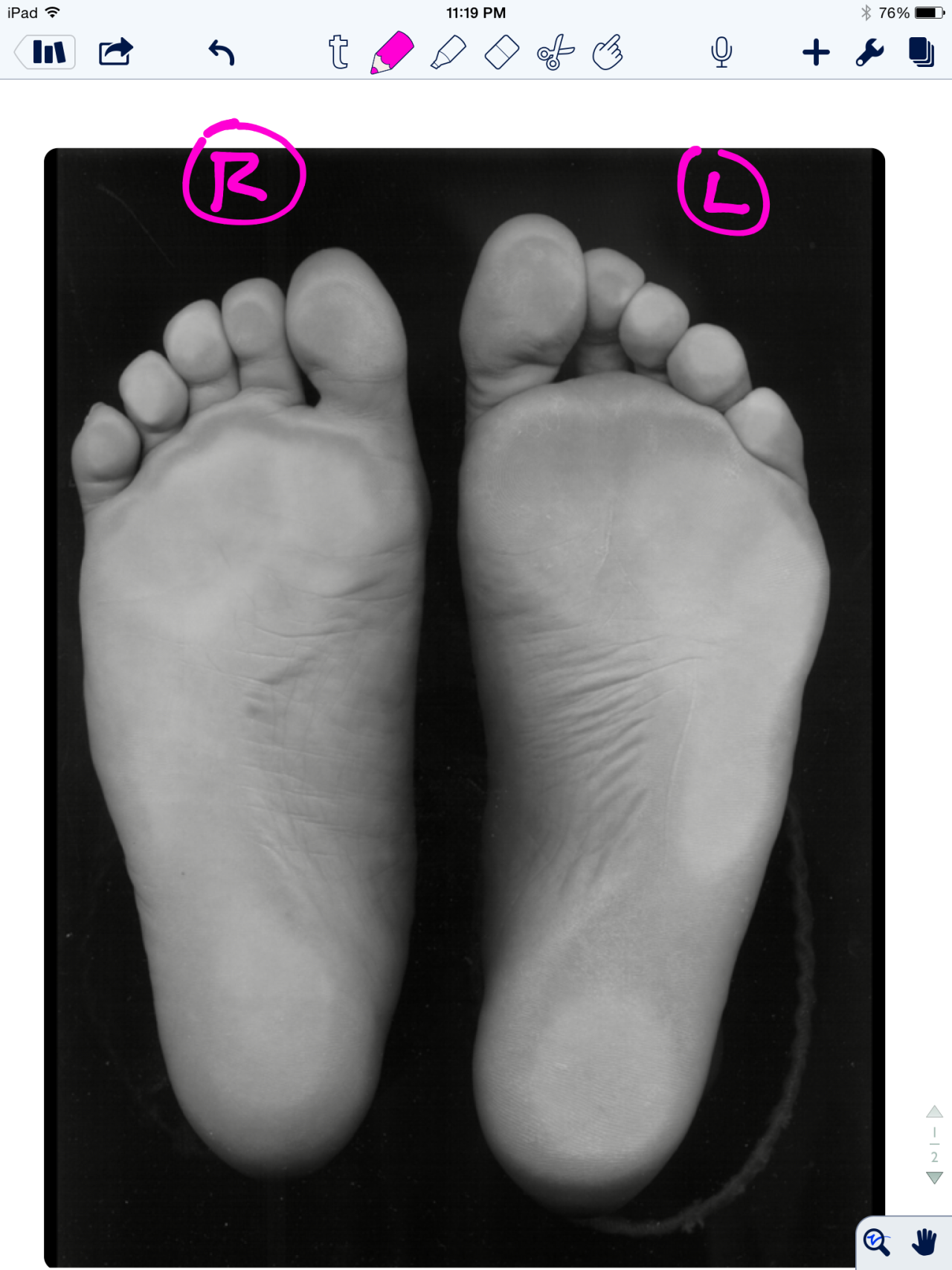
Test your Mental Clinical Thinking Skills with this pedograph case.
A few months ago, we discussed this case in great detail. There is likely little chance you will see our thinking progression with these final conclusions without sitting down with a warm cup of coffee and going over these 2 prior blog posts on this case (part 1 and part 2). Besides, it will be a good review for you and it is great mental gymnastics. This kind of analysis gets easier each time you do it but we have to through out our standard warning. This is the kind of stuff one needs to be able to go through on the fly in one’s practice, it is something to aspire to.
First of all, caveats:
- Our discussions on this case were all theoretical. What we went through was an exercise in static assessment and clinical thinking.
- One cannot, and must not, make clinical decisions from a static assessment.
- As in all assessments, information is taken in, digested and then MUST be confirmed, denied and/or at the very least, folded into a functional and clinically relevant assessment of the client before the findings are accepted, dismissed and acted upon.
- Gait analysis or pedograph-type assessment are helpful tools, but not the final answer.
Our static exam proposal on this case came up with the following theories (please stand up and mimic as we discuss, trust us, it will help you). *Remember: the foot on YOUR LEFT is the RIGHT foot for the purposes of this discussion. And remember, this is all theoretical, this is an exercise in biomechanical and clinical thinking, nothing more.
- Suspect Counter-clockwise pelvis distortion pattern (causes relative internal rotation on LEFT and external rotation on RIGHT), this will drive Left knee hyperextension and Right knee flexion (hence foot plantar pressures as we discussed in previous 2 blog posts linked above). This of course cannot be seen, but we are extrapolating from our clinical experiences.
- poor pronation and internal limb spin control on the left (hence longer foot and toe hammering). Obviously, we would see a dramatic shift of the pressures to the medial foot if this were truly the case. Perhaps this is because of the greater lateral left pelvis drift forcing the glute and foot pronatory controls to have to work harder and longer, and maybe even quicker, to control the internal spin and pronation. Over time, they fatigue and fail rendering a flatter, more pronated and longer heel:toe ball length ratio. This would also give credence to the left toe hammering/gripping response.
- static increased left limb weight bearing (left hip drift)
- abrupt right foot loading pattern (more mid-forefoot strike), perhaps as reflected by the static forefoot loading. Again, supposition.
- with all of the above, it is suspect that this client will appear to have a subtle limp, coming off the left quickly or prematurely as they speed through uncontrolled pronation and resulting in an abrupt right limb loading response that mostly skips through heel strike and results in a more aggressive mid-forefoot loading response. This, sort of, creates a catching of the loading response by the quadriceps more than the gluteals. This can cause medial knee drift (valgus loading) if the medial knee stabilizers are not up to task, this also creates a sudden patellofemoral compresson event and unappreciated sudden tension on the extensor mechanism (the quad-patella-patellar tendon complex). Can you say generic anterior knee pain ?
Just some thoughts. Please go back to the prior 2 blog posts to delve deeper into the conclusions we have brought about here, we have other good reasoning to suspect the above as the scenario. But remember, what you see is not the problem, we see people’s compensations, their strategies. This was just an exercise in “what ifs”, nothing more. But you will see it in your clinic, just substantiate it with an exam, not what you necessarily see in your clients gait or static assessment. Static assessments are for fools, don’t be a fooled fool. What you see is not the problem.
Remember this critical fact. After an injury or a long standing problem, the job of muscles and motor patterns is to stabilize and manage loads (stability and mobility) for adequate and necessary movement. Injuries often leave a mark on the system as a whole because adaptation was necessary during the initial healing phase. This usually spills over during the early movement re-introduction phase, particularly if movement is reintroduced too early or too aggressively. Plasticity is often a culprit. Just because the injury has come and gone does not mean that new patterns of skill, endurance, strength (S.E.S -our favorite mnemonic), stability and mobility were not subsequently built onto the apparently trivial remnants of the injury. There is nothing trivial if it is abnormal. The forces must, and will, play out somewhere in the body and this is often where pain or injury occurs but it is rarely where the underlying problem lives. Is the compensation top down, bottom up, or both ?
Don;t be a fooled fool. Get the facts.
Shawn and Ivo, the gait guys