Premature heel rise: Part 2
/VIDEO: an atypical case of Premature heel rise. A follow up video for yesterdays discussion on the topic.
You should easily see premature heel rise here in this video. We will discuss this case at length with other video projections on our Patreon site next week, if you wish to dive further.
But here you should see, lets focus on the right limb, premature heel rise (again, stick with just watching the right foot/leg). This is, in-part, because this person does not achieve adequate hip extension, you should clearly be able to see that. Loss of terminal hip extension means premature heel rise, no exceptions. Train your eye to see this, you do not need expensive video software to see this.
So, Why inadequate hip extension? Well, just look at the amount of right knee flexion going into terminal stance, it is still heavily flexed and this forces them to prematurely heel rise, avoiding terminal hip extension, and prematurely load the forefoot. Without a knee that extends sufficiently, the hip cannot extend sufficiently, and thus premature heel rise is inevitable. And, trying to solve this issue down at the foot/ankle level is foolish in this case. Stretching this calf day after day until aliens come visit earth will still not be enough stretch time to fix this premature heel rise (ie. get that heel to stay down longer). There is a good reason why this is happening in this person, and it is a neurologic one, one we will discuss on the Patreon site for our Patrons. And, the reason does not matter for the concept I am teaching here today.
For today, you need to be able to see premature heel rise, and know all of the issues behind it, including causes, so that you can direct your phyiscial examination to solve your client's puzzle.
I have included yesterday's post below so you can review and bring this further together.
This is the kind of stuff we will do at Dr. Allen's Friday night Gait Lab, over some beverages. A unique, clinically curious and hungry 25 people need only apply. If you want to get to the next level of your human movement game, this is a way to get there.
Yesterday's post: We know that early/premature heel rise (PHR) leads to premature loading of the forefoot.
We know that premature heel rise (PHR) speeds us through many of the timely mechanical events that need and should occur for to get to safe and effective toe off during walking and running gaits.
This is why there are so many variables that need to be assessed and checked before instituting care to address the premature heel rise, because many times the problem is not even near the heel.
Consider, examine, assess (this is not an exhaustive list either) of causes of PHR
-short calf complex
-short quad (limits hip extension)
- short hip flexors
-anterior pelvis tilt as one's deviated norm posture
- prolonged or excessive rearfoot inversion
-lack of appropriate pronation (sustained supination)
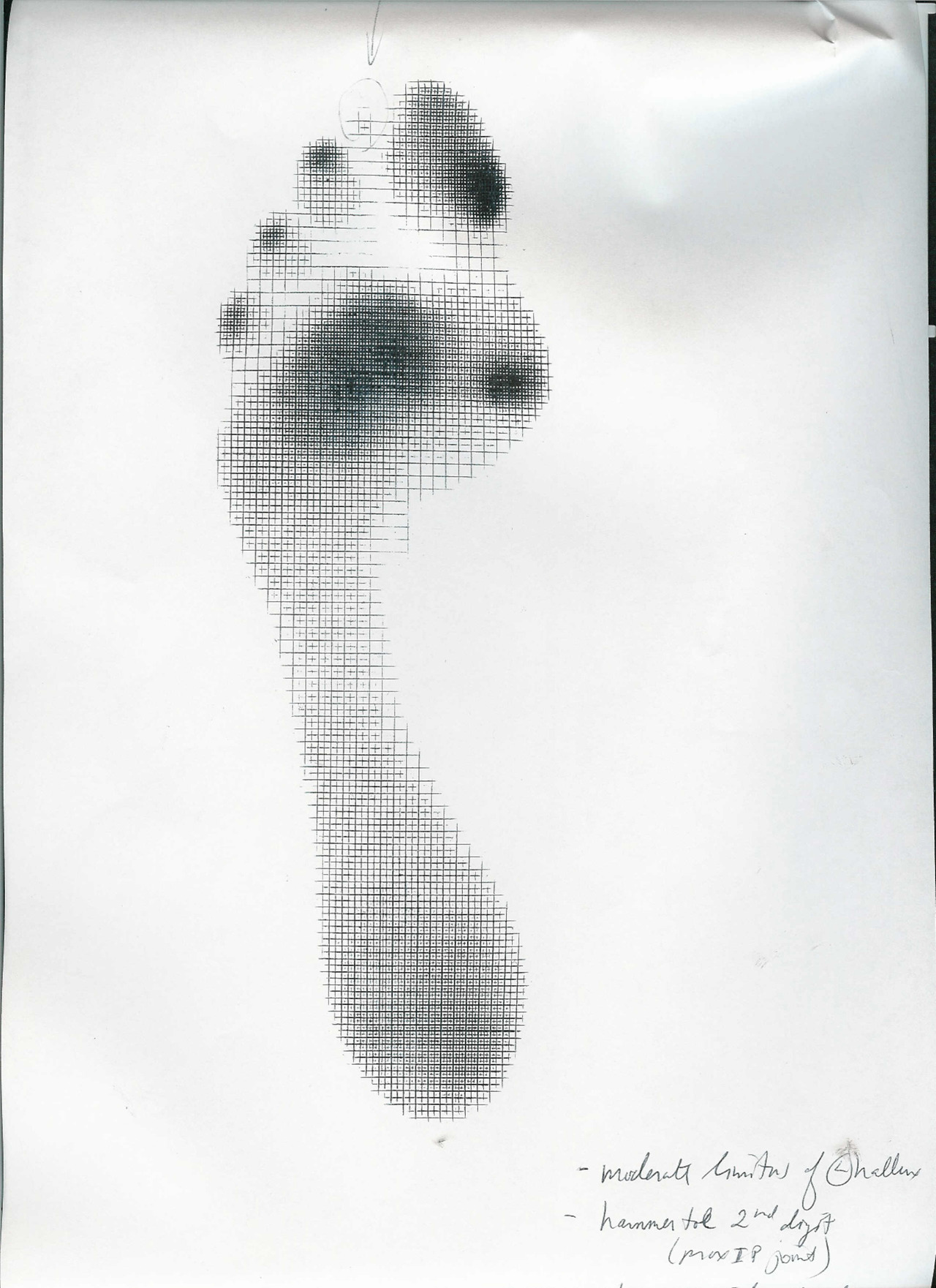
-hallux limitus, rigidus
- weak anterior compartment lower leg
-lack of hip extension/weak glutes
-knee flexion contracture
- neurologic (toe walking gait from youth)
-painful achilles tendon mechanism
- loss of ankle rocker (which has its own long list)
. . . . to name a few
This is why you need to examine your clients, even after a gait analysis. Because, as we like to say, what you see is not your clients gait problem, it is their work around to other mechanical deficits.
After all, telling someone they just need to lengthen/stretch their calf to keep that heel down longer is utterly foolish.
*want to learn more about this stuff, you can join the upcoming Dr. Allen, Friday night Gait Lab series that he will be having in his office one Friday a month, in his Chicagoland office. Stay tuned for that notice. I will take only 25 people per session. We will dive into videos, cases, concepts, white-board rabbit holes, and enjoy some beverages and learn together. Stay tuned. The first 25 to pay and sign up are in !
Shawn Allen, the other gait guy
#gait, #gaitproblems, #gaitanalysis, #heelrise, #PHR, #prematureheelrise, #achilles, #achillestendinitis, #anklerocker, #heelrocker, #forefootpain, #halluxlimitus, #halluxrigidus, #heelpain