We say this so often in our offices.
"You do not have a shoe problem, you have a "thing in the shoe problem", meaning, it is you."
Translation: compromised mechanics leading to tissue overloading.
But we all have to strongly consider that injury is a result of the loading you have not trained gradually into, failure to adapt and accommodate, excessive mileage without adequate tissue recovery,
From the article:
"So Napier and co-author Richard Willy from the University of Montana reviewed the highest-quality research featuring randomized controlled trials and systematic reviews.
"What we see is that there's really no high-level evidence that any running shoe design can prevent injuries," Napier said."
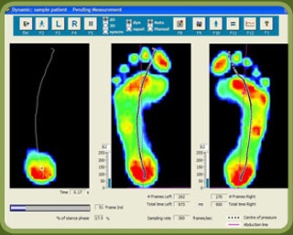
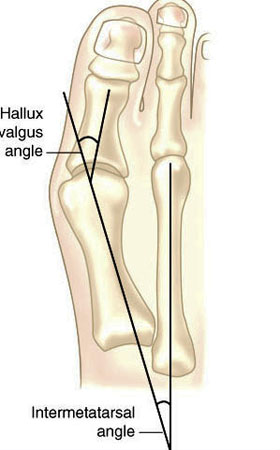
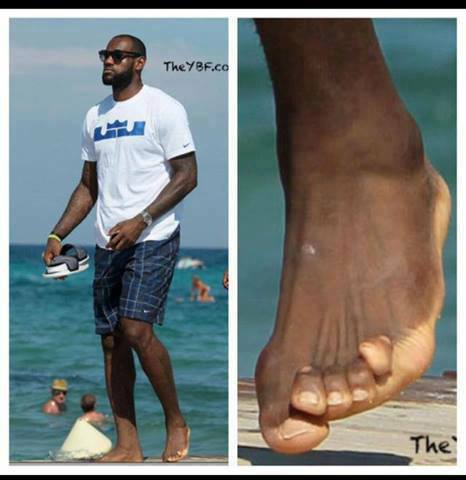
Now, to be honest, in our (the gait guys) opinion, there are times we do recommend a change in the foot wear for a client, and it is often because it appears to be working against someone mechanics and is a contributory factor in their injury or complaint. And sometimes that shoe recommendation is a temporary one, and sometimes a permanent one. We can use a shoe to help us get to a better/faster end point. After all, when we sprain an ankle sometime a brace or crutches are helpful and protective, of temporary value. A wisely chosen shoe can act the same if we are dealing with an acute achilles tendinopathy or a painful bunion for example. And in those cases we might recommend a shoe that can give us an assist. Sometime, when appropriate perhaps it is a shoe with a stronger medial post, perhaps one with a higher or lower heel drop/delta, or more or less stack height, or perhaps a mid/forefoot rocker built into the shoe. The truth is, people come in with functional or "fixed" pathology and sometimes pairing up a shoe to help us around some conflicting biomechanics can be temporarily, and sometimes permanently, helpful. But, the shoe is never the only answer, a wise clinician has many things they can utilize, all the way up the kinetic chain sometimes.
The more you know, the better you can assist someone.
Shawn Allen, one of the gait guys
#Nigg, #barefoot, #shoes, #stackheight, #heeldrop, #achillestendinitis, #bunion, #pronation, #supination, #running, #gait, #thegaitguys, #gaitanalysis, #gaitproblems, #gaitcompensation
Can the design of a running shoe help prevent injury? A B.C. researcher says he has the answer
Kelly Crowe · CBC News · Posted: Dec 15, 2018 9:00 AM ET
https://www.cbc.ca/news/health/running-shoe-injury-prevention-second-opinion-1.4947408?fbclid=IwAR3XaGPdgfQ68wj2N0tHqIamDdpYuxTIIL2LeudUd-doYN8YqQrIZI9-s9E