Rearfoot to Hip Pathomechanical considerations.
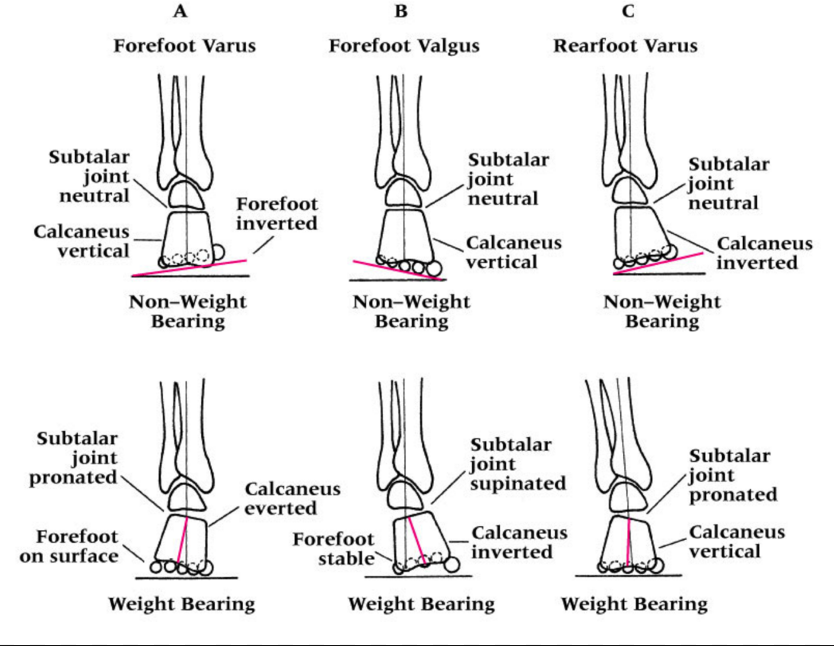
In normal gait, the rearfoot strikes in slight inversion and then quickly moves through eversion in the frontal plane to help with the midfoot through forefoot pronation phases of gait. Some sources would refer this rearfoot eversion as the rearfoot pronatory phase, after all. pronation can occur at the rear, mid or forefoot. As with all pronation in all areas, when it occurs too fast, too soon or too much, it can be a problem and rearfoot eversion is no different. If uncontrolled via muscles such as through tibialis posterior eccentric capabilities (Skill, endurance, strength) or from a structural presentation of Rearfoot Valgus pain can arise.
From a scenario like in the video above, where a more rearfoot varus presentation is observed, where the lateral to medial pronation progression is excessive and extreme in terms of speed, duration and magnitude this can also create too much lateral to medial foot, ankle and knee movement. This will often accompany unchecked movements of internal spin through the hip. So one should see that these pronation and spin issues can occur and be controlled from the bottom or from the top, and hopefully adequately from both in a normal scenario. It is when there is a biomechanical limitation or insufficiency somewhere in the chain that problems can arise. And remember, pain does not have to occur where the failure occurs, in fact it usually does not. So when you have knee pain from an apparent valgus posturing knee, make sure you look above and below that knee. Also, keep in mind that as discussed last week in the blog post on ischiofemoral impingment syndrome (link), these spin scenarios can be quite frequently found with ipsilateral frontal plane lateral deviations (bumping of the hip-pelvis outside the vertical stacking of the foot-knee-hip stacking line). This stacking failure can also be the source of many of the issues discussed above, so be sure you are looking locally and globally. And remember, what you see is not the problem, it is their compensation around their deeper problem quite often.
If you have not read the blog post from last week on ischiofemoral impingement syndrome you might not know where the components of the cross over gait come in to play here nor how a rearfoot problem can present with a hip impingement scenario, so I can recommend that article one more time.
One last thing, just in case you think this stuff is easy to work through, remember that these rearfoot varus and valgus problems, and pronation rates. and limb spin rates are all highly variable when someone has varying degrees of femoral torsion, tibial torsion or talar torsion. Each case is different, and each will be unique in their presentation and in the uniqueness of the treatment recipe. I just thought I would throw that in to make your head spin a little in case it wasn’t already.
For example, a case where the rearfoot is a semi rigid varus, with tibial varum, and frontal plane lateral pelvic drift with components of cross over gait (ie. the video case above) will require a different treatment plan and strategy than the same rearfoot varus in a presentation of femoral torsion challenges and genu valgum. Same body parts, different orientations, different mechanics, different treatment recipe.
So, you can fiddle with a dozen pair of shoes to find one that helps minimize your pains, you can go for massages and hope for the best, you can go and get activated over and over, you can try yet another new orthotic, you can go to a running clinic and try some form changes, throw in some yoga or pilates, compression wear, voodoo bands and gosh who knows what else. Sometimes they are the answer or stumble across it … or you can find someone who understands the pieces of the puzzle and how to piece a reasonable recipe together to bake the cake just right. We do not always get there, but we try.
Want more ? Try our National Shoe Fit certification program for a starter or try our online teleseminars at www.onlinece.com (we did a one hour course on the RearFoot just the other night, and it was recorded over at onlineCE.com).
Dr. Shawn Allen, of the gait guys
Reference:
Man Ther. 2014 Oct;19(5):379-85. doi: 10.1016/j.math.2013.10.003. Epub 2013 Oct 29.Clinical measures of hip and foot-ankle mechanics as predictors of rearfoot motion and posture. Souza TR et al.
Health professionals are frequently interested in predicting rearfoot pronation during weight-bearing activities. Previous inconsistent results regarding the ability of clinical measures to predict rearfoot kinematics may have been influenced by the neglect of possible combined effects of alignment and mobility at the foot-ankle complex and by the disregard of possible influences of hip mobility on foot kinematics. The present study tested whether using a measure that combines frontal-plane bone alignment and mobility at the foot-ankle complex and a measure of hip internal rotation mobility predicts rearfoot kinematics, in walking and upright stance. Twenty-three healthy subjects underwent assessment of forefoot-shank angle (which combines varus bone alignments at the foot-ankle complex with inversion mobility at the midfoot joints), with a goniometer, and hip internal rotation mobility, with an inclinometer. Frontal-plane kinematics of the rearfoot was assessed with a three-dimensional system, during treadmill walking and upright stance. Multivariate linear regressions tested the predictive strength of these measures to inform about rearfoot kinematics. The measures significantly predicted (p ≤ 0.041) mean eversion-inversion position, during walking (r(2) = 0.40) and standing (r(2) = 0.31), and eversion peak in walking (r(2) = 0.27). Greater values of varus alignment at the foot-ankle complex combined with inversion mobility at the midfoot joints and greater hip internal rotation mobility are related to greater weight-bearing rearfoot eversion. Each measure (forefoot-shank angle and hip internal rotation mobility) alone and their combination partially predicted rearfoot kinematics. These measures may help detecting foot-ankle and hip mechanical variables possibly involved in an observed rearfoot motion or posture.