The case of the lateral thigh, leg and knee pain
/note how the bottom of the heel cup is rounded
This gal came to see us with pain in the lateral thigh, knee, and lateral lower leg on the left. It has happened recently with skiing and alleviated only temporarily with acupuncture of the vastus lateralis and peroneal groups. She has been skiing with a foot bed (please see picture).
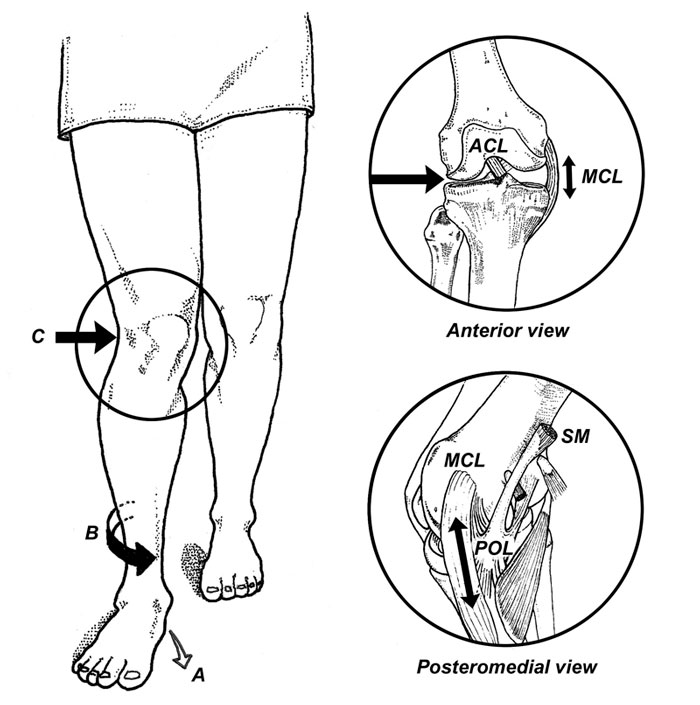
Evaluation reveals mild bilateral external tibial torsion, a right anatomically short leg tibial, and bilateral medial knee fall (knee is medial of the sagittal plane) L>R during weight-bearing when the feet are pointing straight ahead. There is moderate loss of the medial longitudinal arches bilaterally, greater on the left.
We remember that when a patient has external tibial torsion, when the knees points straight the feet point to the outside.
Translated to skiing, the feet need to be straightahead which brings the knee(s) inside of the sagittal plane.
We remember that often times with leg length discrepancy is, the longer leg side will “pronate ” in attempt to shorten extremity and the shorter leg side “supinate”, in an attempt to lengthen the extremity.
Putting this all together: the patient is pronating bilaterally, left greater than right with medial knee fall. The ski shop put the footbed you see in the picture in both of the patients boots. You can see that it is extremely rounded at the heel and, because orthotics are shank dependent devices, a round heel like this will just roll into pronation as there is more weight on the medial longitudinal arch. This makes the entire foot bed assembly relatively ineffective and increases the valgus moment at the knee, stressing the vastus lateralis as it is trying to pull the knee to midline as well as the peroneal group as it is trying to do the same from a closed chain position as well as supinate the foot.
We placed a 3 mm sole lift under the right foot and added a post to the bottom the left orthotic to allow it to sit flat. This did not correct the problem completely and we needed to add a Morton’s toe extension (post under the first metatarsal) to invert the foot and bring the knee out into the sagittal plane.
Dr Ivo Waerlop, one of The Gait Guys
#footbeds #kneepain #orthotics #skibootfit #thighpain #legpain #quadriceps