The Case of the Curly Toes
/Here, we talk about one common reason you may see a unilateral increase in long flexor tone.
Here, we talk about one common reason you may see a unilateral increase in long flexor tone.

We talk about triangles a lot. Think about triangles. Hey Pythaogoras did! They are powerful distributors of force. Here we will talk about 3 of them.
There are 4 layers of muscles in the foot. The 1st triangle occurs in the 1st layer. Think of the abductor hallucis and the abductor digiti minimi. Proximally they both attach to the calcaneus and distally to the 1st and 5th proximal phalanges. Now think about the transverse metatarsal ligament that runs between the disal metatarsal heads. Wow, a triangle! this one is superficial.
Now think about the adductor hallicus. It has a transverse and oblique head. think about that transverse metatarsal ligament again. Wow, another triangle!
What about the flexor hallicus brevis and flexor digiti minimi? The former originates from the cuboid, lateral cunieform andd portion of the tib posterior tendon; the latter from the proximal 5th metatarsal. They both go forward and insert into the respective proximal phalynx (with the sesamoids intervening in the case of the FHB). and what connects these? The deep transverse metatarsal ligament of course! And this triangle surrounds the adductor triangle, with both occurring the 3rd layer of the 4 layers of foot muscles.
Triangles… and you thought geometry was boring!
Remaining triangular when we need to (because of our pointy heads)…
Here we look at genu valgus in kids. What she needs to know and how to keep track of it.
No, not how does the gait SOUND, but can they hear? We have long payed attention to the mechanics of gait, muscles and proprioception, and many times, if you have been following us for any length of time, the interplay of all three. But how often have you considered someones hearing in your evaluation?
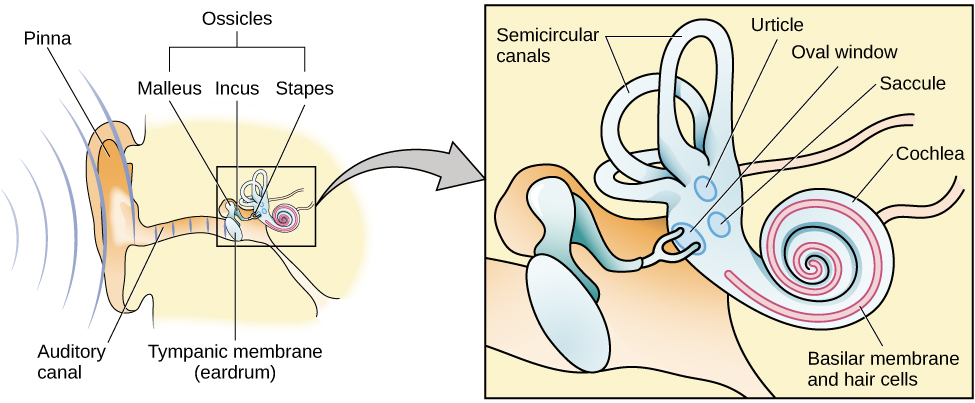
Anatomically, the hearing organs (hair cells, otolithic apparatus, cochlea) are conveniently located right next store to the vestibular system (utricle, saccule and semicircular canals). The hearing organs start with mechanical vibrations of the tympanic membrane (ear drum) which move 3 auditory bones (or ossicles) called the incus, malleus and stapes. The vibrations move the stapes moves in and out of the fluid filled cochlea and vibrate crystals laying on a platform (otolith) in which hair cells are imbedded and if the vibration sufficient, the nerves attached to the hair cells fire and you can hear your favorite baseline by Cliff Williams (or Cliff Burton, John Myung, Bootsy Collins or whomever you like to listen to).
The vestibular system, as you probably know, monitors position and velocity of movement of the head. There are three hula hoop type structures called “semicircular canals” (see picture above) that monitor rotational and tilt position and angular acceleration, as well as two other structures, the utricle and saccule, which monitor tilt and linear acceleration.
The vestibular apparatus (the canals and the utricle and saccule) feed into a part of the brain called the floccular nodular lobe of the cerebellum, which as we are sure you can imagine, have something to do with balance and coordination. This area of the cerebellum feeds back to the vestibular system (actually the vestibular nucleii); which then feed back up to the brain as well as (you guessed it) down the spinal cord and to predominantly the extensor muscles.
Can you see how the 2 systems are “attached” to one another and could conceivably be interrelated? When you move fluid in one system (endo or peri lymph) you HAVE to move fund in the other. The fluid displaces, (like air, in air filled shoes or insoles), it does not deform (like EVA in an insole)
It is well established that hearing impaired folks (especially kids) have gait (and often balance) problems (1-3) and the worse the hearing loss, the worse the gait disturbance (1). This can occur in middle aged (4), as well as older adults as well (5-7). Perhaps this is due to viscosity changes in the endo or perilymph (8), otosclerosis of the ossicles (9,10) or other age related changes in utricle and saccule function (5-7). Also, for the 1st time, we are documenting a “sensory reweighting” which occurs when auditory cues are changed (4), with a greater reliance on visual cues. Hmmm. We wonder how this plays out with listening to music while walking or running?
So, The next time someone you see has a gait or balance problem, check their hearing and adjust your treatment program accordingly : )
References:
1. Melo RS. Gait performance of children and adolescents with sensorineural hearing loss.
Gait Posture. 2017 Jun 3;57:109-114. doi: 10.1016/j.gaitpost.2017.05.031.
2. Jafarnezhadgero AA, Majlesi M, Azadian E. Gait ground reaction force characteristics in deaf and hearing children. Gait Posture. 2017 Mar;53:236-240. doi: 10.1016/j.gaitpost.2017.02.006. Epub 2017 Feb 14.
3. Janky KL, Givens D.Vestibular, Visual Acuity, and Balance Outcomes in Children With Cochlear Implants: A Preliminary Report. Ear Hear. 2015 Nov-Dec;36(6):e364-72. doi: 10.1097/AUD.0000000000000194.
4. Maheu M, Sharp A, Landry SP, Champoux F. Sensory reweighting after loss of auditory cues in healthy adults. Gait Posture. 2017 Mar;53:151-154. doi: 10.1016/j.gaitpost.2017.01.015. Epub 2017 Jan 24.
5. Agmon M, Lavie L, Doumas M. The Association between Hearing Loss, Postural Control, and Mobility in Older Adults: A Systematic Review. J Am Acad Audiol. 2017 Jun;28(6):575-588. doi: 10.3766/jaaa.16044. Review.
6. Layman AJ1, Li C, Simonsick E, Ferrucci L, Carey JP, Agrawal Y. Association Between Saccular Function and Gait Speed: Data From the Baltimore Longitudinal Study of Aging. Otol Neurotol. 2015 Jan 7. [Epub ahead of print]
7. Otol Neurotol. 2012 Jul;33(5):832-9. doi: 10.1097/MAO.0b013e3182545061.
Decline in semicircular canal and otolith function with age.
Agrawal Y1, Zuniga MG, Davalos-Bichara M, Schubert MC, Walston JD, Hughes J, Carey JP.
8. Wu T, Marcus DC. Age-Related Changes in Cochlear Endolymphatic Potassium and Potential in CD-1 and CBA/CaJ Mice . JARO: Journal of the Association for Research in Otolaryngology. 2003;4(3):353-362. doi:10.1007/s10162-002-3026-6.
9. Grayeli AB1, Sterkers O, Toupet M. Audiovestibular function in patients with otosclerosis and balance disorders. Otol Neurotol. 2009 Dec;30(8):1085-91. doi: 10.1097/MAO.0b013e3181b0fd5d.
10. Ozmen AO1, Aksoy S, Ozmen S, Saraç S, Sennaroğlu L, Gürsel B. Balance after stapedotomy: analysis of balance with computerized dynamic posturography. Clin Otolaryngol. 2009 Jun;34(3):212-7. doi: 10.1111/j.1749-4486.2009.01915.x.
Key tag words:
running, gait, injuries, kidney, kidneydamage, marathoners, foot, feet, dehydration, heatstroke, elon musk, neural lace, hip pain, crossfit, squats, deadlifts, LLD, short leg, dystonia, runner's dystonia, posture,
Summary: Today we hit some very important topics on how to examine a client and how asymmetries play into gait, running, posture and pathomechanics. We hope you enjoy today's show, it is our first one back in 6 weeks. We are back strong after a brief early summer sabbatical. Back to the "podcast every 2 weeks" again. Thanks for being patient while Ivo recharged for the second half of the year. Plus, on today's show, we also dive into Runner's kidney, dehydration, gluteal gripping, runner's dystonia, functional leg length differences due to asymmetries, and more !
Show links:
http://traffic.libsyn.com/thegaitguys/pod_124final.mp3
http://thegaitguys.libsyn.com/pod-124
Our Websites:
www.thegaitguys.com
summitchiroandrehab.com doctorallen.co shawnallen.net
Our website is all you need to remember. Everything you want, need and wish for is right there on the site.
Interested in our stuff ? Want to buy some of our lectures or our National Shoe Fit program? Click here (thegaitguys.com or thegaitguys.tumblr.com) and you will come to our websites. In the tabs, you will find tabs for STORE, SEMINARS, BOOK etc. We also lecture every 3rd Wednesday of the month on onlineCE.com. We have an extensive catalogued library of our courses there, you can take them any time for a nominal fee (~$20).
Our podcast is on iTunes, Soundcloud, and just about every other podcast harbor site, just google "the gait guys podcast", you will find us.
Show Notes:
Kidney Damage in Runners. 82% !?
http://www.newsweek.com/running-bad-you-marathons-damage-kidneys-runners-bodies-575829
Kidney nephropathy in mesoamericans.
http://www.ajkd.org/article/S0272-6386(15)01257-3/fulltext
Elon Musk's Neural Lace.
https://www.scoopwhoop.com/elon-musk-launches-neuralink-which-hopes-to-combine-your-brain-with-artificial-intelligence/
Leg length discrepancies,do they really even exist ?
Dystonia ?
The Gluteal gripping phenomenon.

Less pain through better mechanics?
We have been using toe separators for various foot problems like hallux valgus, hammer toes and flexor dominance/extensor weakness. Our reasoning is that through changing the angle of attachment of the muscle, you alter the mechanical advantage of that muscle and help it to work more efficiently. This seems implied in the literature with respect to foot orthoses (1-3) but we could not find any data regarding toe separators. Toe separators DO seem to reduce pain and increase function (4-6). Perhaps this is through better biomechanics, mechanical deformation, proprioceptive changes, or most likely a combination of all these factors and more. We think clinical results speak volumes. It is nice to see more data coming out on these easy to implement clinical tools.
What is you clinical reasoning or rationale for using these devices? We would love to hear and if you have an article for reference you could share, that would be great.
TGG
1. Scherer PR, Sanders J, Eldredge DE, Duffy SJ, Lee RY. Effect of functional foot orthoses on first metatarsophalangeal joint dorsiflexion in stance and gait. J Am Podiatr Med Assoc. 2006 Nov-Dec;96(6):474-81.
2. Halstead J, Chapman GJ, Gray JC, Grainger AJ, Brown S, Wilkins RA, Roddy E, Helliwell PS, Keenan AM, Redmond ACFoot orthoses in the treatment of symptomatic midfoot osteoarthritis using clinical and biomechanical outcomes: a randomised feasibility study. Clin Rheumatol. 2016 Apr;35(4):987-96. doi: 10.1007/s10067-015-2946-6. Epub 2015 Apr 28.
3. Bishop C, Arnold JB, May T. Effects of Taping and Orthoses on Foot Biomechanics in Adults with Flat-Arched Feet. Med Sci Sports Exerc. 2016 Apr;48(4):689-96. doi: 10.1249/MSS.0000000000000807.
4. Chadchavalpanichaya N, Prakotmongkol V, Polhan N, Rayothee P, Seng-Iad S. Effectiveness of the custom-mold room temperature vulcanizing silicone toe separator on hallux valgus: A prospective, randomized single-blinded controlled trial. Prosthet Orthot Int. 2017 Mar 1:309364617698518. doi: 10.1177/0309364617698518. [Epub ahead of print]
5. Tehraninasr A, Saeedi H, Forogh B, Bahramizadeh M, Keyhani MR. Effects of insole with toe-separator and night splint on patients with painful hallux valgus: a comparative study. Prosthet Orthot Int. 2008 Mar;32(1):79-83. doi: 10.1080/03093640701669074.
6. Tang SF, Chen CP, Pan JL, Chen JL, Leong CP, Chu NK. The effects of a new foot-toe orthosis in treating painful hallux valgus. Arch Phys Med Rehabil. 2002 Dec;83(12):1792-5.
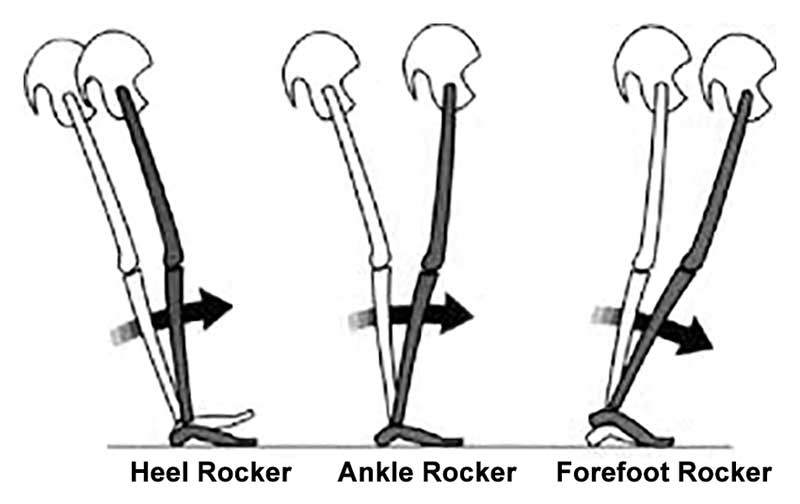
How many times have we talked about ankle rocker and its importance? So how are YOU measuring ankle rocker? Are you looking at it on the table? On the ground? Weight bearing? Knee flexed or extended (or both?). The knee is extended at initial contact, flexes through midstance, extends at terminal stance and pre swing and flexes again during swing phase until extending at the end of terminal swing for initial contact again.
What you see on the table may not (and many times doesn't) translate to real life. Someone with limited ankle dorsiflexion non weight bearing may have normal amounts during gait and vice versa. With gravity in place and a functioning (or malfunctioning) vestibular system, things can change rapidly. Remember that the vestibular system drives the extensors and if inhibited, you will often have flexor dominance. Talk about a tight gastroc/soleus group!
"These findings indicate that nonweightbearing and weightbearing measurements of ankle DF PROM with knee extension should not be used interchangeably and that weightbearing ankle DF PROM with the knee extended is more appropriate for estimating ankle DF during gait."
Kang MH, Oh JS. Relationship Between Weightbearing Ankle Dorsiflexion Passive Range of Motion and Ankle Kinematics During Gait. J Am Podiatr Med Assoc. 2017 Jan;107(1):39-45. doi: 10.7547/14-112.
"There is no relationship between a static diagnosis of ankle dorsiflexion at 0° with dorsiflexion during gait. On the other hand, those subjects with less than -5° of dorsiflexion during static examination did exhibit reduced ankle range of motion during gait."
Gatt A, De Giorgio S, Chockalingam N, Formosa C. A pilot investigation into the relationship between static diagnosis of ankle equinus and dynamic ankle and foot dorsiflexion during stance phase of gait: Time to revisit theory? Foot (Edinb). 2017 Mar;30:47-52. doi: 10.1016/j.foot.2017.01.002. Epub 2017 Feb 6.

"too much tripping, soles worn thin.... too much trippin and my souls worn thin"
Scott Weiland: Stone Temple Pilots
Nothing earth shattering here. Tripping (no, not THAT kind) can be due to many variables including biomechanical as well as alterations in surfaces and/or terrain. For probable proprioceptive reasons and less brain "interpolation", walking slower decreases your trip risk. This study looked at minimal clearance of the great toe (requiring adequate ankle dorsiflexion as well as great toe dorsiflexion). This was classically used to determine trip risk. This new measure called the "trip risk integral" calculates stability throughout the gait cycle rather than just a single point in time.
The results?
"... slower gait is both an important covariate and potential intervention for trip-related falls."
our conclusion: Look at the WHOLE gait cycle, not just at one point intime...
Schulz BW A new measure of trip risk integrating minimum foot clearance and dynamic stability across the swing phase of gait. J Biomech. 2017 Apr 11;55:107-112. doi: 10.1016/j.jbiomech.2017.02.024. Epub 2017 Feb 27.
We often find clinically that the quadratus femoris as becoming the 1st dysfunctional muscle of the deep 6 external rotators (1) and its pain referral pattern can mimic the piriformis (2) and piriformis syndrome (3) as well as hamstring insertional tendinitis. It has also been implicated in some cases of femoroacetabular impingement (4) as well as ishiofemoral impingement (5). It is active during walking stance phase, and moreso during stance while running as well as with a clamshell exercise with external rotation (6). It appears to be maximally lengthened with flexion and adduction or abduction, with internal rotation ( a great position of you need to stretch this muscle), and is deducted to be strongest going from a 60-90 degree flexed position into extension (ie: it has the with the largest moment arms observed for extension in the deduced force-length efficient range of 60-90° flexion)(7).
Needling this muscle can sometimes pose a challenge. Here is a demo of one way to accomplish it I often employ while needling some of the other surrounding hip musculature.
Consider the QF the next time you have someone with hamstring insertional pain, or diffuse hip pain that you are having a difficult time localizing.
Dalmau-Carolà J Myofascial pain syndrome affecting the quadratus femoris Pain Pract. 2010 May-Jun;10(3):257-60. doi: 10.1111/j.1533-2500.2009.00347.x. Epub 2010 Feb 11
Diamond LE, Van den Hoorn W, Bennell KL, Wrigley TV, Hinman RS, O'Donnell J, Hodges PW. Coordination of deep hip muscle activity is altered in symptomatic femoroacetabular impingement. J Orthop Res. 2016 Aug 11. doi: 10.1002/jor.23391. [Epub ahead of print]
Semciw, Adam I. et al. Quadratus femoris: An EMG investigation during walking and running Journal of Biomechanics , Volume 48 , Issue 12 , 3433 - 3439
Vaarbakken K, Steen H, Samuelsen G, Dahl HA, Leergaard TB, Stuge B .Primary functions of the quadratus femoris and obturator externus muscles indicated from lengths and moment arms measured in mobilized cadavers. Clin Biomech (Bristol, Avon). 2015 Mar;30(3):231-7. doi: 10.1016/j.clinbiomech.2015.02.004. Epub 2015 Feb 11.
Rockered footwear is for more than Hallux Limitus..

To go along with yesterdays post on Hallux Limitus... In case you missed it, click here
In other words, footwear with more "drop" in the front lessens the need for forefoot rocker (otherwise known as 1st metatarsophalangeal joint extension, or "the ability to bend your big toe backward)
“Most people have to wear MBTs a little at a time until they gain strength and stamina, so we recommend wearing them an hour a day for the first few days and to increase gradually until they feel strong enough to wear them for a full day,”
...sounds an awful lot like our mantra "skill, endurance, strength"...
A great read here. Keep this one around for reference...
http://lermagazine.com/article/rocker-bottom-footwear-effects-on-balance-gait
#rockeredshoe #rocker #footwear
Hallux Limitus. Today on Case in One Minute


Genu valgum in kids: What you need to know
We have all seen this. The kid with the awful “knock knees”. It is a Latin word “which means “bent” or “knock kneed”. It appears to have 1st been used in 1884.
This condition, where the Q angle angle exceeds 15 degrees, usually presents maximally at age 3 and should resolve by age 9. It is usually physiologic in development due to obliquity of the femur, when the medial condyle is lower than the lateral. Normal development and weight bearing lead to an overgrowth of the medial condyle of the femur. This, combined with varying development of the medial and lateral epiphysies of the tibial plateau leads to the valgus development. Gradually, with increased weight bearing, the lateral femoral condyle (and thus the tibial epiphysis) bear more weight and this appears to slow, and eventually reverse the valgum.
Normal knee angulation usually progresses from 10-15 degrees varus at birth to a maximal valgus angle of 10-15 degreesat 3-3.5 years (see picture). The valgus usually decreases to an adult angle of 5-7 degrees. Remember that in women, the Q angle should be less than 22 degrees with the knee in extension and in men, less than 18 degrees. It is measured by measuring the angle between the line drawn from the ASIS to the center of the patella and one from the center of the patella through the tibial tuberosty, while the leg is extended.
Further evaluation of a child is probably indicated if:
Management is by serial measurement of the intermalleolar distance (the distance between ankles when the child’s knee are placed together) to document gradual spontaneous resolution (hopefully). If physiologic genu valgum persists beyond 7-8 years of age, an orthopaedic referral would be indicated but certainly intervention with attempts at corrective exercises and gait therapy should be employed. Persistence in the adult can cause a myriad of gait, foot, patello femoral and hip disorders, and that is the topic on another post.
Promotion of good foot biomechanics through the use of minimally supportive shoes, encouraging walking on sand (time to take that trip to the beach!), walking on uneven surfaces (like rocks, dirt and gravel), gentle massage (to promote muscle facilitation for those muscles which test weak (origin/insertion work) and circulation), gait therapeutic exercises and acupuncture when indicated, can all be helpful.

Like to run in Zero Drop shoes? Good... we do too... but look at this:
"Barefoot running induced higher loading rates during overground running than the highest drop condition, while it was the opposite during treadmill running. Ankle plantar flexion and knee flexion angles at touchdown were higher during treadmill than overground running for all conditions, except for barefoot which did not show any difference between the tasks."
So, if you want to reduce vertical loading rates, run barefoot on a treadmill.
Does this mean if we want to decrease vertical loading rates when running overground (NOT on a treadmill) we should run in shoes with a large drop?
It seems, according to this study, that kinematics are the same with barefoot but not with shoes.
Which is best for you? You decide...
http://link.springer.com/article/10.1007%2Fs00421-014-3072-x

There are several mechanisms in place to stabilize the medial foot tripod. Some, we would hope many in fact, would argue that the process starts up in the glutes in controlling the rate of internal rotation of the limb during the weight bearing response. The glute has to help slow down that spin, hopefully to the point that when the knee reaches its sagittal tracking plane, the spin stops. And, if the knee stops its inward course, the tibia will stop spinning and thus excessive pronation loads into the foot tripod.
Jumping past a bunch of other variables here, for the sake of a shorter article, many typically feel that the tibialis posterior and peroneal sling is additionally important and cannot be ignored. Then there is a concept we pound hard here on TGG, that one must have adequate control of the rate, speed, degree of pronation. Again, that comes in part from the sling we just mentioned and of course the skill, endurance and strength of the anterior compartment components, mostly the toe extensors and tibialis anterior. Their eccentric control slows the forefoot loading and thus controls the rate and degree of foot tripod splay/collapse. If too weak /too fatigued will render too much splay and too much pronation for too long. All this, and of course other components (too many to get into here today) when insufficient will create a differential in rotation and bending/flexing loads into the tibia, classically presenting at the distal third of the tibia where Medial Tibial Stress Syndrome (MTSS) classically takes root.
We have discussed many times, here on the blog and on our 100+ podcasts about having a competent foot tripod for a given loading response. Specifically addressing the medial tripod, because this is classically where the foot tripod fails, this anchoring of the medial foot tripod around the 1st metatarsophalangeal joint can only occur if there is a harmonious activation of the long and short flexors and extensors of the hallux, and predicated on a proper plantarflexion of the 1st metatarsal to procure proper orientation and purchase of the metatarsal head on the surface/ground not to mention a competent foot tripod.
This study, investigated and determined some curious findings of linking a history of MTSS with increased isometric FHL (flexor hallucis longus) strength. Namely, they felt that when there was a history of MTSS, it resulted in increased FHL isometric strength.
Why might this be pre-predictive in our mind ? Well, hammering the big toe into aggressive flexion will act to help synergistically stabilize the medial foot tripod, and thus assist in pronation control even though it is not a primary optimal strategy. This scenario, thought clearly not an optimal strategy, rather a compensation, often sets up global toe gripping strategies, and as we have discussed long ago, a strong link to subungal hematomas (black toenail, bleeding under the toe nails. (link:https://thegaitguys.tumblr.com/post/6355488304/the-black-plague-ok-kinda-sort-ofsubungal). However, to be fair, as mentioned at the end of this article, the authors of the study in question felt that the increased FHL might be from an attempt to make up for weakened FDL to the lesser toes. If you are looking for it, someone who has an incompetent medial foot tripod, will often hammer the big toe down while sometime completely disabling the 1st metatarsal purchase on the ground. I have termed these clients as "knuckle poppers" because they cannot find the medial tripod, and their attempts are from over-recruitment of the long hallux flexor (FHL). The problem here in lies that one cannot properly toe off the big toe, which should be in extension, when they were still just in a FHL life or death strategy. This can set up a functional hallux limitus. Often, someone with such a functionally troubled medial tripod strategy, will toe off more laterally, choosing not to drive through the medial tripod and hallux, merely because they cannot do so well.
"In this study, the MVIC torque of the 1st MTPJ plantar flexion was significantly higher in runners with a history of MTSS than without it."
"Our results suggest that runners with a history of MTSS adopt a strategy of reducing the load to the medial tibia because of their history of MTSS."
This may be the case in some, but i am not sure we entirely agree this is the case. We are trying to postulate that the failed tripod is more likely. Meaning, more uncontrolled medial loading of the foot and thus increased load to the medial tibia. This leans towards this articles comment that,
"A previous study reported that excessive pronation during motion is a risk factor of developing MTSS [9, 11]. The results also suggest that the FDL and TP muscles that act to support the arch of the foot tend to be stressed in runners who potentially have a risk for developing MTSS. On the other hand, although the FHL, which is an agonist of 1st MTPJ plantar flexion, has a function similar to those of the FDL and TP as the inversion muscle of the ankle, FHL is not likely to be related to development of MTSS because the FHL does not connect to tibial fascia [22]. "
We would suggest that, it does not have to connect to the tibial fascia to be a relevant issue. It is about the loads directly and indirectly across the tibia, not the actual connections.
However, we do not argue with their statement,
"Thus, this characteristic increase in MVIC torque of the 1st MTPJ in runners with a history of MTSS could be considered to be a result of increased activity of the FHL to avoid pain caused by contraction stress of the FDL, which could be a possible cause of MTSS." But, what we are suggesting is that perhaps the increased FHL is not to avoid the pain, but an attempt to help stabilize the medial foot tripod.
Two interesting side notes/thoughts from this article are,
"Collectively, muscle strength characteristics in runners with a history of MTSS could be considered to be a result of increasing activity of the FHL to reduce the load on FDL and avoid pain caused by contraction stress of the FDL."
"A previous study reported that the FHL tendon branches to the 2nd and 3rd toe in most cases [24]. Therefore, it could be considered that the absence of a significant difference in the MVIC torques of the 2nd–5th MTPJ between runners with and without a history of MTSS could be due to the effects of the branching of FHL tendon to the 2nd and 3rd toe."
This investigators did admit some possible limitations in this study, one of which was "we investigated the relationships between MTSS and muscle strength as a static assessment. Therefore, it is unclear whether the results directly reflect muscle endurance or activity during running. "
- the gait guys
Reference:
Ankle and toe muscle strength characteristics in runners with a history of medial tibial stress syndrome
Junya Saeki
Masatoshi Nakamura,
Sayaka Nakao,
Kosuke Fujita,
Ko Yanase,
Katsuyuki Morishita and
Noriaki Ichihashi
https://jfootankleres.biomedcentral.com/articles/10.1186/s13047-017-0197-2
Join us in this brief video about tibial torsion and genu valgum in a 6-year-old
Mooney JF 3rd Lower extremity rotational and angular issues in children. Pediatr Clin North Am. 2014 Dec;61(6):1175-83. doi: 10.1016/j.pcl.2014.08.006. Epub 2014 Sep 18.
Killam PE. Orthopedic assessment of young children: developmental variations. Nurse Pract. 1989 Jul;14(7):27-30, 32-4, 36.
Kling TF Jr, Hensinger RN. Angular and torsional deformities of the lower limbs in children. Clin Orthop Relat Res. 1983 Jun;(176):136-47.
Key tag words:
foot types, rearfoot, forefoot, pronation, supination, shoe fit, forefoot varus, forefoot supinatus, rearfoot inversion, ankle rocker, injuries, rehab, corrective exercises
Rearfoot varus and Rearfoot valgus. Knowing the anatomy of your rear foot and its anatomic and functional posturing can lead to many problems in anyone. If you do not know the rearfoot type and posturing, you will not understand the rest of the foot mechanics. Without this knowledge, you will not know the reason for midfoot or forefoot problems, not understand what shoe you are in, or even why the shoe, footbed, orthotic you have chosen is either not fixing your problems, or causing them. Join us on a journey down the rearfoot rabbit hole over the next hour. Plus a few funny stories to lighten the biomechanics-heavy dialogue.
Show links:
http://traffic.libsyn.com/thegaitguys/pod_123final_cut.mp3
http://thegaitguys.libsyn.com/podcast-123-the-rear-foot-understanding-your-rearfoot-type
Show sponsors:
www.newbalancechicago.com
www.thegaitguys.com
That is our website, and it is all you need to remember. Everything you want, need and wish for is right there on the site.
Interested in our stuff ? Want to buy some of our lectures or our National Shoe Fit program? Click here (thegaitguys.com or thegaitguys.tumblr.com) and you will come to our websites. In the tabs, you will find tabs for STORE, SEMINARS, BOOK etc. We also lecture every 3rd Wednesday of the month on onlineCE.com. We have an extensive catalogued library of our courses there, you can take them any time for a nominal fee (~$20).
Our podcast is on iTunes, Soundcloud, and just about every other podcast harbor site, just google "the gait guys podcast", you will find us.
Show Notes:
https://www.ncbi.nlm.nih.gov/pubmed/27134364
https://www.ncbi.nlm.nih.gov/pubmed/25364132
RearFoot positions:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3588658/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3990938/
Powers CM, Maffucci R, Hampton S. Rearfoot posture in subjects with patellofemoral pain. J Orthop Sports Phys Ther. 1995 Oct;22(4):155-60.
Power V, Clifford AM. The Effects of Rearfoot Position on Lower Limb Kinematics during Bilateral Squatting in Asymptomatic Individuals with a Pronated Foot Type. J Hum Kinet. 2012 Mar;31:5-15. doi: 10.2478/v10078-012-0001-0. Epub 2012 Apr 3.
Shultz SP, Song J, Kraszewski AP, Hafer JF, Rao S, Backus , Mootanah R, Hillstrom HJ. An Investigation of Structure, Flexibility and Function Variables that Discriminate Asymptomatic Foot Types. J Appl Biomech. 2016 Dec 19:1-25. [Epub ahead of print]

Geee....Looks like forefoot rocker really IS IMPORTANT, eh?
...and what have we been saying about being able to dorsiflex your big toe? Watch how well you or your client can descend the 1st ray (remember that if the head of the 1st does not go down and anchor, its axis of rotation moves dorsally and posterior, limiting dorsiflexion of the joint)
This article should make you look at the "toe break" in a shoe...
"They found that increasing bending stiffness assisted with propulsion during running, reducing the metabolic cost of running by about 1%. However, at a certain level, the increased elasticity began to interfere with the natural flexion of the first MTP joint, reducing the contribution of ankle joint torque to push-off and counteracting the metabolic benefits. Within the study population, the threshold of bending stiffness for optimal energetics varied significantly from one runner to the next, suggesting running shoe design may need to be tuned to an individual runner’s needs."
http://lermagazine.com/news/in-the-moment-sports-medicine/stiffer-shoes-improve-running-energetics-as-long-as-first-mtp-flexion-is-preserved
Metatarsus Adductus: The Basics


A few points to remember:
1. Bleck E: Metatarsus adductus: classification and relationship to outcomes of treatment. J Pediatric Orthop 3:2-9,1983.
2. Bohne W. Metatarsus adductus. Bulletin of the New York Academy of Medicine. 1987;63(9):835-838. link to FREE full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1629274/
3. http://www.wheelessonline.com/ortho/metatarsus_adductus
4. Peabody, C.W. and Muro, F.: Congenital metatarsus varus. J. Bone Joint Surg. 15:171-89, 1933.
5. Truslow, W.: Metatarsus primus varus or hallux valgus? J. Bone Joint Surg.23:98-108, 1925.
6. Jacobs J: Metatarsus varus and hip dysplasia. C/inO rth o p 16:203-212, 1960
additional references:
Kane R. Metatarsus varus. Bulletin of the New York Academy of Medicine. 1987;63(9):828-834. link to FREE full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1629282/
Wynne-Davies R, Littlejohn A, Gormley J. Aetiology and interrelationship of some common skeletal deformities. (Talipes equinovarus and calcaneovalgus, metatarsus varus, congenital dislocation of the hip, and infantile idiopathic scoliosis). Journal of Medical Genetics. 1982;19(5):321-328. link to FREE full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1048914/
What is going on with this gal? Hmmmmm.... Watch on...

Plantar thermal stress response (TSR) leads to skin shear forces.
"Fifteen eligible subjects were enrolled. The left foot was used as a reference and fitted to a self-adjusted and habitual lace-tightening method by each subject. The right foot was used as a test closure and fitted into three lace closure conditions: loose, tight, and preset optimal closure (reel clutch, BOA technology). Thermal images were taken after 5 minutes of acclimatization (pre-trial) and immediately after 200 walking steps in each shoe closure condition (post-trial)."
Their conclusions:
"The results from this study suggest that shoelace closure technique can have a profound effect on TSR. It therefore stands to reason that optimal lace closure may have an impact in reducing risk of plantar ulcers in people with Diabetic peripheral neuropathy (DPN). Interestingly, results revealed that even a self-adjusted lace closure may not be necessarily optimal and a preset closure setting like reel clutch might ultimately be recommended to minimize risk."
Lace Up for Healthy Feet: The Impact of Shoe Closure on Plantar Stress Response
Hadi Rahemi, PhD, David G. Armstrong, DPM, MD, PhD, Ana Enriquez, BSc, Joshua Owl,BSc, Talal K. Talal, DPM, Bijan Najafi, PhD, MSc
First Published April 18, 2017
http://journals.sagepub.com/doi/abs/10.1177/1932296817703669?platform=hootsuite&journalCode=dsta
OUR SEARCH BOX IS INTUITIVE, TYPE IN YOUR KEY WORD, WAIT, THEN SCROLL DOWN.
Email us: our email is found under the "Disclaimer" Tab above.
Powered by Squarespace.