What? Gait and hearing....
/No, not how does the gait SOUND, but can they hear? We have long payed attention to the mechanics of gait, muscles and proprioception, and many times, if you have been following us for any length of time, the interplay of all three. But how often have you considered someones hearing in your evaluation?
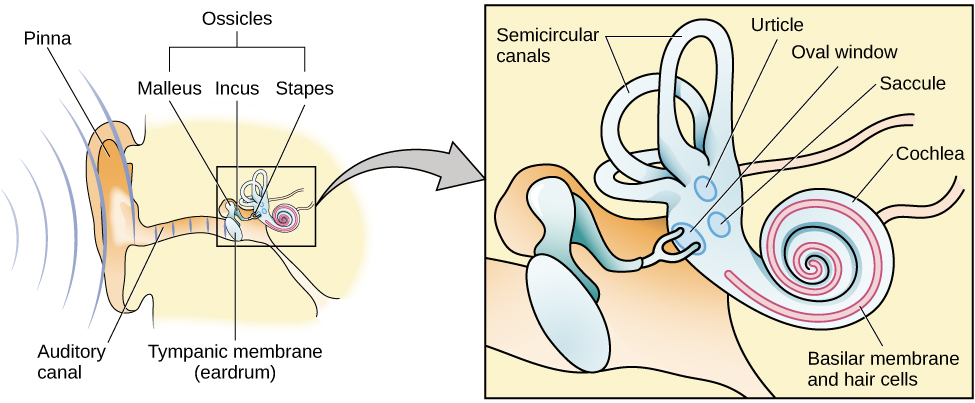
Anatomically, the hearing organs (hair cells, otolithic apparatus, cochlea) are conveniently located right next store to the vestibular system (utricle, saccule and semicircular canals). The hearing organs start with mechanical vibrations of the tympanic membrane (ear drum) which move 3 auditory bones (or ossicles) called the incus, malleus and stapes. The vibrations move the stapes moves in and out of the fluid filled cochlea and vibrate crystals laying on a platform (otolith) in which hair cells are imbedded and if the vibration sufficient, the nerves attached to the hair cells fire and you can hear your favorite baseline by Cliff Williams (or Cliff Burton, John Myung, Bootsy Collins or whomever you like to listen to).
The vestibular system, as you probably know, monitors position and velocity of movement of the head. There are three hula hoop type structures called “semicircular canals” (see picture above) that monitor rotational and tilt position and angular acceleration, as well as two other structures, the utricle and saccule, which monitor tilt and linear acceleration.
The vestibular apparatus (the canals and the utricle and saccule) feed into a part of the brain called the floccular nodular lobe of the cerebellum, which as we are sure you can imagine, have something to do with balance and coordination. This area of the cerebellum feeds back to the vestibular system (actually the vestibular nucleii); which then feed back up to the brain as well as (you guessed it) down the spinal cord and to predominantly the extensor muscles.
Can you see how the 2 systems are “attached” to one another and could conceivably be interrelated? When you move fluid in one system (endo or peri lymph) you HAVE to move fund in the other. The fluid displaces, (like air, in air filled shoes or insoles), it does not deform (like EVA in an insole)
It is well established that hearing impaired folks (especially kids) have gait (and often balance) problems (1-3) and the worse the hearing loss, the worse the gait disturbance (1). This can occur in middle aged (4), as well as older adults as well (5-7). Perhaps this is due to viscosity changes in the endo or perilymph (8), otosclerosis of the ossicles (9,10) or other age related changes in utricle and saccule function (5-7). Also, for the 1st time, we are documenting a “sensory reweighting” which occurs when auditory cues are changed (4), with a greater reliance on visual cues. Hmmm. We wonder how this plays out with listening to music while walking or running?
So, The next time someone you see has a gait or balance problem, check their hearing and adjust your treatment program accordingly : )
References:
1. Melo RS. Gait performance of children and adolescents with sensorineural hearing loss.
Gait Posture. 2017 Jun 3;57:109-114. doi: 10.1016/j.gaitpost.2017.05.031.
2. Jafarnezhadgero AA, Majlesi M, Azadian E. Gait ground reaction force characteristics in deaf and hearing children. Gait Posture. 2017 Mar;53:236-240. doi: 10.1016/j.gaitpost.2017.02.006. Epub 2017 Feb 14.
3. Janky KL, Givens D.Vestibular, Visual Acuity, and Balance Outcomes in Children With Cochlear Implants: A Preliminary Report. Ear Hear. 2015 Nov-Dec;36(6):e364-72. doi: 10.1097/AUD.0000000000000194.
4. Maheu M, Sharp A, Landry SP, Champoux F. Sensory reweighting after loss of auditory cues in healthy adults. Gait Posture. 2017 Mar;53:151-154. doi: 10.1016/j.gaitpost.2017.01.015. Epub 2017 Jan 24.
5. Agmon M, Lavie L, Doumas M. The Association between Hearing Loss, Postural Control, and Mobility in Older Adults: A Systematic Review. J Am Acad Audiol. 2017 Jun;28(6):575-588. doi: 10.3766/jaaa.16044. Review.
6. Layman AJ1, Li C, Simonsick E, Ferrucci L, Carey JP, Agrawal Y. Association Between Saccular Function and Gait Speed: Data From the Baltimore Longitudinal Study of Aging. Otol Neurotol. 2015 Jan 7. [Epub ahead of print]
7. Otol Neurotol. 2012 Jul;33(5):832-9. doi: 10.1097/MAO.0b013e3182545061.
Decline in semicircular canal and otolith function with age.
Agrawal Y1, Zuniga MG, Davalos-Bichara M, Schubert MC, Walston JD, Hughes J, Carey JP.
8. Wu T, Marcus DC. Age-Related Changes in Cochlear Endolymphatic Potassium and Potential in CD-1 and CBA/CaJ Mice . JARO: Journal of the Association for Research in Otolaryngology. 2003;4(3):353-362. doi:10.1007/s10162-002-3026-6.
9. Grayeli AB1, Sterkers O, Toupet M. Audiovestibular function in patients with otosclerosis and balance disorders. Otol Neurotol. 2009 Dec;30(8):1085-91. doi: 10.1097/MAO.0b013e3181b0fd5d.
10. Ozmen AO1, Aksoy S, Ozmen S, Saraç S, Sennaroğlu L, Gürsel B. Balance after stapedotomy: analysis of balance with computerized dynamic posturography. Clin Otolaryngol. 2009 Jun;34(3):212-7. doi: 10.1111/j.1749-4486.2009.01915.x.