There are several mechanisms in place to stabilize the medial foot tripod. Some, we would hope many in fact, would argue that the process starts up in the glutes in controlling the rate of internal rotation of the limb during the weight bearing response. The glute has to help slow down that spin, hopefully to the point that when the knee reaches its sagittal tracking plane, the spin stops. And, if the knee stops its inward course, the tibia will stop spinning and thus excessive pronation loads into the foot tripod.
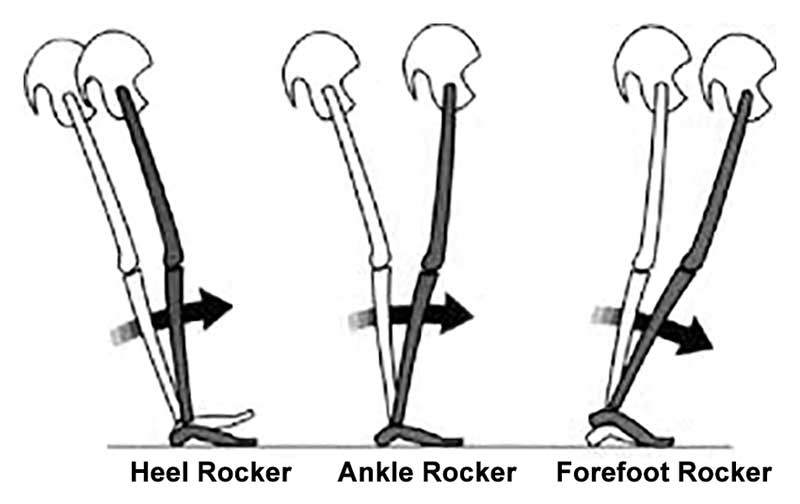
Jumping past a bunch of other variables here, for the sake of a shorter article, many typically feel that the tibialis posterior and peroneal sling is additionally important and cannot be ignored. Then there is a concept we pound hard here on TGG, that one must have adequate control of the rate, speed, degree of pronation. Again, that comes in part from the sling we just mentioned and of course the skill, endurance and strength of the anterior compartment components, mostly the toe extensors and tibialis anterior. Their eccentric control slows the forefoot loading and thus controls the rate and degree of foot tripod splay/collapse. If too weak /too fatigued will render too much splay and too much pronation for too long. All this, and of course other components (too many to get into here today) when insufficient will create a differential in rotation and bending/flexing loads into the tibia, classically presenting at the distal third of the tibia where Medial Tibial Stress Syndrome (MTSS) classically takes root.
We have discussed many times, here on the blog and on our 100+ podcasts about having a competent foot tripod for a given loading response. Specifically addressing the medial tripod, because this is classically where the foot tripod fails, this anchoring of the medial foot tripod around the 1st metatarsophalangeal joint can only occur if there is a harmonious activation of the long and short flexors and extensors of the hallux, and predicated on a proper plantarflexion of the 1st metatarsal to procure proper orientation and purchase of the metatarsal head on the surface/ground not to mention a competent foot tripod.
This study, investigated and determined some curious findings of linking a history of MTSS with increased isometric FHL (flexor hallucis longus) strength. Namely, they felt that when there was a history of MTSS, it resulted in increased FHL isometric strength.
Why might this be pre-predictive in our mind ? Well, hammering the big toe into aggressive flexion will act to help synergistically stabilize the medial foot tripod, and thus assist in pronation control even though it is not a primary optimal strategy. This scenario, thought clearly not an optimal strategy, rather a compensation, often sets up global toe gripping strategies, and as we have discussed long ago, a strong link to subungal hematomas (black toenail, bleeding under the toe nails. (link:https://thegaitguys.tumblr.com/post/6355488304/the-black-plague-ok-kinda-sort-ofsubungal). However, to be fair, as mentioned at the end of this article, the authors of the study in question felt that the increased FHL might be from an attempt to make up for weakened FDL to the lesser toes. If you are looking for it, someone who has an incompetent medial foot tripod, will often hammer the big toe down while sometime completely disabling the 1st metatarsal purchase on the ground. I have termed these clients as "knuckle poppers" because they cannot find the medial tripod, and their attempts are from over-recruitment of the long hallux flexor (FHL). The problem here in lies that one cannot properly toe off the big toe, which should be in extension, when they were still just in a FHL life or death strategy. This can set up a functional hallux limitus. Often, someone with such a functionally troubled medial tripod strategy, will toe off more laterally, choosing not to drive through the medial tripod and hallux, merely because they cannot do so well.
"In this study, the MVIC torque of the 1st MTPJ plantar flexion was significantly higher in runners with a history of MTSS than without it."
"Our results suggest that runners with a history of MTSS adopt a strategy of reducing the load to the medial tibia because of their history of MTSS."
This may be the case in some, but i am not sure we entirely agree this is the case. We are trying to postulate that the failed tripod is more likely. Meaning, more uncontrolled medial loading of the foot and thus increased load to the medial tibia. This leans towards this articles comment that,
"A previous study reported that excessive pronation during motion is a risk factor of developing MTSS [9, 11]. The results also suggest that the FDL and TP muscles that act to support the arch of the foot tend to be stressed in runners who potentially have a risk for developing MTSS. On the other hand, although the FHL, which is an agonist of 1st MTPJ plantar flexion, has a function similar to those of the FDL and TP as the inversion muscle of the ankle, FHL is not likely to be related to development of MTSS because the FHL does not connect to tibial fascia [22]. "
We would suggest that, it does not have to connect to the tibial fascia to be a relevant issue. It is about the loads directly and indirectly across the tibia, not the actual connections.
However, we do not argue with their statement,
"Thus, this characteristic increase in MVIC torque of the 1st MTPJ in runners with a history of MTSS could be considered to be a result of increased activity of the FHL to avoid pain caused by contraction stress of the FDL, which could be a possible cause of MTSS." But, what we are suggesting is that perhaps the increased FHL is not to avoid the pain, but an attempt to help stabilize the medial foot tripod.
Two interesting side notes/thoughts from this article are,
"Collectively, muscle strength characteristics in runners with a history of MTSS could be considered to be a result of increasing activity of the FHL to reduce the load on FDL and avoid pain caused by contraction stress of the FDL."
"A previous study reported that the FHL tendon branches to the 2nd and 3rd toe in most cases [24]. Therefore, it could be considered that the absence of a significant difference in the MVIC torques of the 2nd–5th MTPJ between runners with and without a history of MTSS could be due to the effects of the branching of FHL tendon to the 2nd and 3rd toe."
This investigators did admit some possible limitations in this study, one of which was "we investigated the relationships between MTSS and muscle strength as a static assessment. Therefore, it is unclear whether the results directly reflect muscle endurance or activity during running. "
- the gait guys
Reference:
Ankle and toe muscle strength characteristics in runners with a history of medial tibial stress syndrome
Junya Saeki
Masatoshi Nakamura,
Sayaka Nakao,
Kosuke Fujita,
Ko Yanase,
Katsuyuki Morishita and
Noriaki Ichihashi
https://jfootankleres.biomedcentral.com/articles/10.1186/s13047-017-0197-2