Podcast 167: Is symmetry important for biomechanics and energy utilization?
/Podcast 167: Is symmetry important for biomechanics and energy utilization? Plus, things that mimic plantar fasciitis. Including trigger points you never thought might be implicated.
This podcast is way more interesting than the title !
join us each month on the Masterclass in Gait
https://www.patreon.com/thegaitguys
Join at the $40 monthly level and get the masterclass each month, bonus material and the detailed monthly content we only share on Patreon.
The Masterclass is a formal LIVE presentation of slides, videos, demos, deep dives on topics you will not hear anywhere but here ! We hit the gait, biomechanics, neurology and orthopedics of all of the gait topics we present. This is not for the weak and timid, this is the deep dive you have been waiting for. Join us while we turn our normal 50 minute presentations into 3.5 hours on a regular basis ! The 40$ Patreon level will give you the Masterclass and also get you the $20, $10, and 5$ Patreon level content. What a deal ! It will not be here forever so lock in now !
Or, you can get less for your money (why would you do that?) and just buy our Monthly $40 Masterclass at our VIMEO on demand page: https://vimeo.com/ondemand/thegaitmasterclass
Links to find the podcast:
Look for us on Apple Podcasts, Google Play, Podbean, PlayerFM, RADIO and more.
Just Google "the gait guys podcast".
_______________________________________________________________________________
Our Websites:
www.thegaitguys.com
Find Exclusive content at: https://www.patreon.com/thegaitguys
doctorallen.co
summitchiroandrehab.com
shawnallen.net
Our website is all you need to remember. Everything you want, need and wish for is right there on the site.
Interested in our stuff ? Want to buy some of our lectures or our National Shoe Fit program? Click here (thegaitguys.com or thegaitguys.tumblr.com) and you will come to our websites. In the tabs, you will find tabs for STORE, SEMINARS, BOOK etc. We also lecture every 3rd Wednesday of the month on onlineCE.com. We have an extensive catalogued library of our courses there, you can take them any time for a nominal fee (~$20).
Our podcast is on iTunes and just about every other podcast harbor site, just google "the gait guys podcast", you will find us.
Where to find us, the podcast Links:
Apple podcasts:
https://itunes.apple.com/us/podcast/the-gait-guys-podcast/id559864138?mt=2
Google Play:
https://play.google.com/music/m/Icdfyphojzy3drj2tsxaxuadiue?t=The_Gait_Guys_Podcast
Links for today's show:
https://traffic.libsyn.com/secure/thegaitguys/167_Dec_4_2020_.mp3
https://thegaitguys.libsyn.com/is-symmetry-important-for-biomechanics-and-energy-utilization
https://directory.libsyn.com/episode/index/id/17322929
Association between trigger points in hamstring, posterior leg, foot muscles and plantar fasciopathy: A cross- sectional study
J Bodyw Mov Ther. 2020 Oct;24(4):373-378. doi: 10.1016/j.jbmt.2020.07.018. Epub 2020 Aug 7. Ravindra C Thummar 1 , Sannasi Rajaseker 2 , Ranjith Anumasa 3
https://physoc.onlinelibrary.wiley.com/doi/abs/10.1113/JP280509
Journal of Physiology.
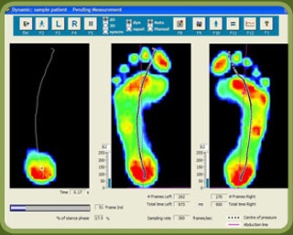
The human preference for symmetric walking often disappears when one leg is constrained
Michael G. Browne, Cameron S. Smock, Ryan T. Roemmich, Nov 24, 2020