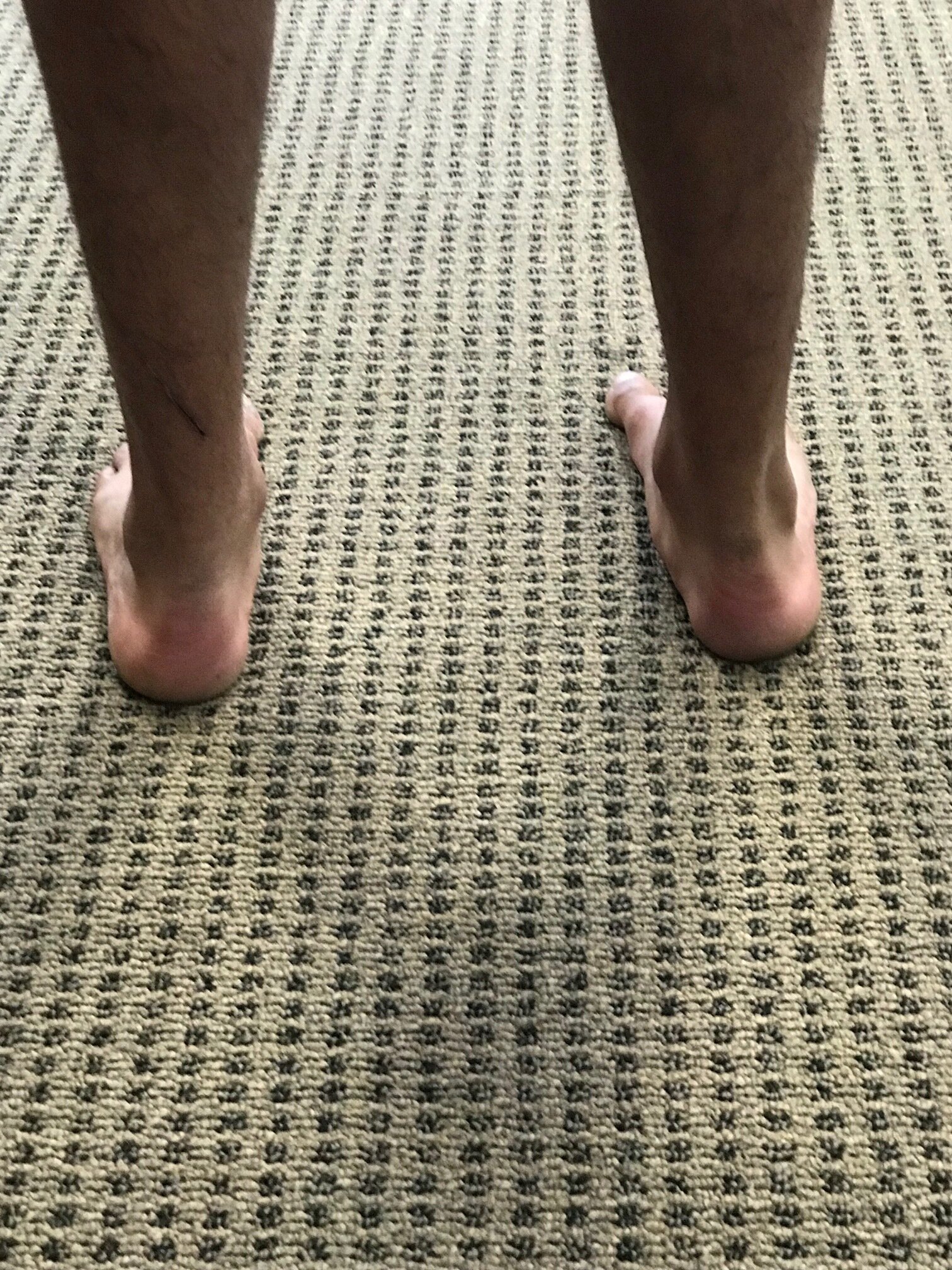
Unilateral calcaneal valgus: what can it mean?
/right calcaneal valgus
Take a good look at this picture and what do you see? Do you see the calcaneal valgus on the right side. What runs through your mind?
Possibilities for causing this condition, as well as the clinical implications are numerous.
The short list should include:
A shorter leg on the contralateral side: often times we will pronate more on the longer leg side to compensate for a short leg on the opposite
Increased rear foot and/or fore foot pronation on the valgus side. Laxity of the spring ligament or incompetency of the musculature which helps to maintain your arch (tibialis posterior, foot intrinsics, tibialis anterior to name a few) often causes more collapse on the effected side
A lack of available rearfoot eversion on the contralateral side. It may be that the increase calcaneovalgus is normal and the opposite side is more rigid.
If you were seeing this in the middle of the gait cycle it could be that that is their strategy to get around a loss of hip extension or ankle rocker
External tibial torsion on that side. Go ahead, stand up and spin your right foot into external rotation and keep your left foot with a normal progression angle. Can you see how your arch collapses to a greater degree on the side with the external torsion? Remember that pronation is dorsiflexion, eversion and abduction.
Internal tibial torsion on the contralateral side. Internal tibial torsion puts the foot into supination which makes it into more of a rigid lever rather than mobile adapter.
And the list goes on…
Next time you see a unilateral deformity like this, hopefully some of these things run through your mind and will help you to pinpoint where the problem actually is.
Dr Ivo Waerlop, one of The Gait Guys
#calcanealeversion #rearfootvalgus
#lowerextremitydeformities