The “Standing on Glass” Static Foot/Pedograph Assessment: Part 1
/The “Standing on Glass” Static Foot/Pedograph... PART 1
We hope you find this case presentation dialogue interesting.
* note: This is a static assessment dialogue. One cannot, and must not, make clinical decisions from a static assessment. As in all assessments, information is taken in, digested and them MUST be confirmed, denied and/or at the very least, folded into a functional and clinically relevant assessment of the client before the findings are accepted, dismissed and acted upon.
The “Standing on Glass” Static Foot/Pedograph Assessment: Part 1
* note: This is a static assessment dialogue. One cannot, and must not, make clinical decisions from a static assessment. As in all assessments, information is taken in, digested and them MUST be confirmed, denied and/or at the very least, folded into a functional and clinically relevant assessment of the client before the findings are accepted, dismissed and acted upon. As we always say, a gait analysis or pedograph-type assessment is never enough to make decisions on treatment to resolve problems and injuries. What is seen and represented on either are the client’s strategies around clinical problems or compensations. Today’s photo and blog post are an exercise in critical clinical thinking to get the juices flowing and to get the observer thinking about the client’s presentation and to help open up the field to questions the observer should be entertaining. The big questions should be, “why do i see this, what could be causing these observances ?”
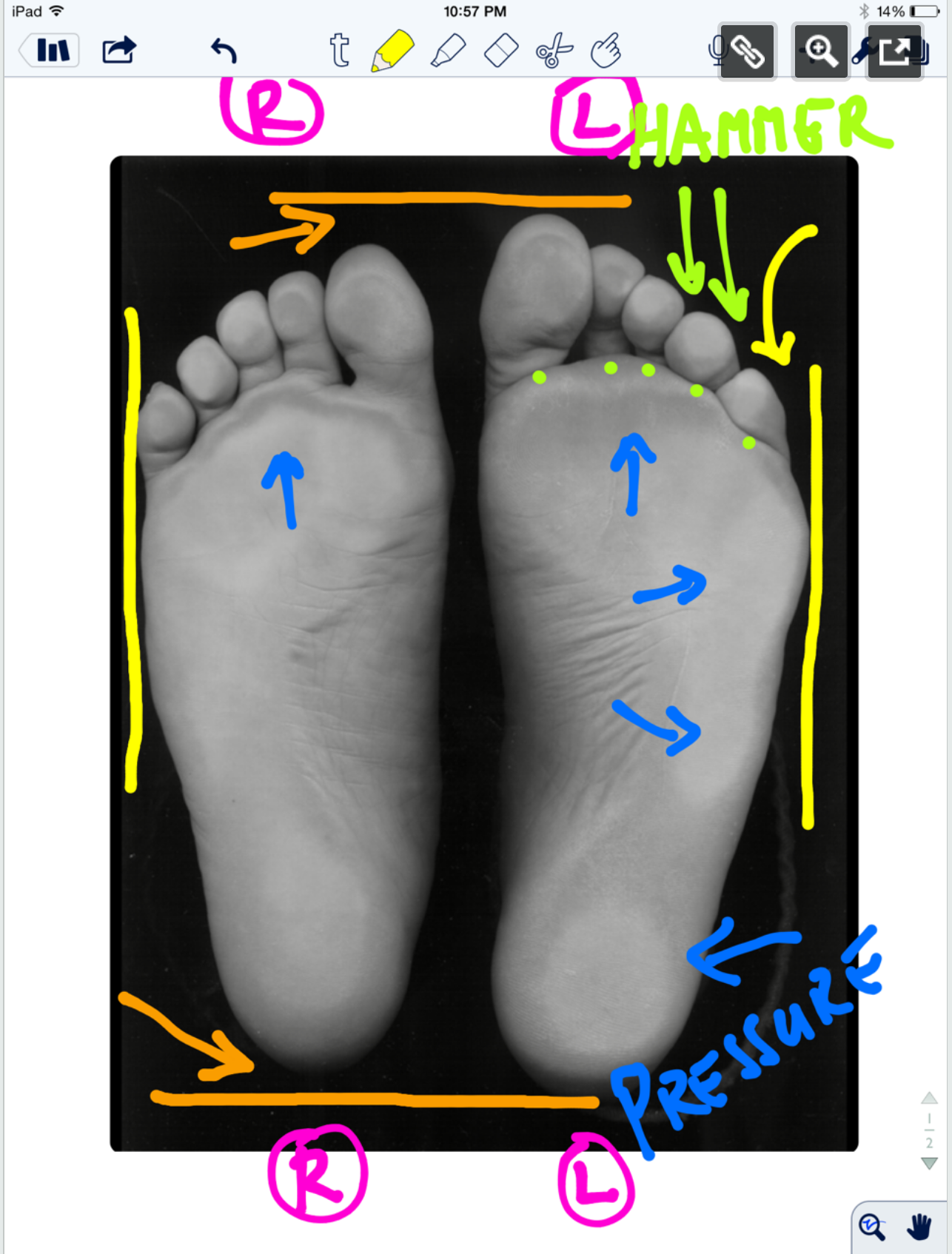
* note the right and left sides by the R and L circled in pink.
ORANGE lines: The right foot appears to be shorter, or is it that the left is longer (see the lines and arrows drawing your attention to these differences)? A shorter foot could be represented by a supinated foot (if you raise the arch via the windlass mechanism you will shorten the foot distance between the rear and forefoot). A longer foot could be represented by a more pronated foot. Is that what we have here ? There is no way to know, this is a static presentation of a client standing on glass. What we should remember is that the goal is always to get the pelvis square and level. If an anatomically or functionally short leg is present, the short leg side MAY supinate to raise the mortise and somewhat lengthen the leg. In that same client, they may try to meet the process part way by pronating the other foot to functionally “shorten” that leg. Is that what is happening here ? So, does this client have a shorter right leg ? Longer left ? Do you see a plunking down heavily onto the right foot in gait ? Remember, what you see is their compensation. Perhaps the right foot is supinating, and thus working harder at the bottom end of the limb (via more supination), to make up for a weak right glute failing to eccentrically control the internal spin of the leg during stance phase ? OR, perhaps the left foot is pronating more to drive more internal rotation on the left limb because there is a restricted left internal hip rotation from the top ? Is the compensation top-down or bottom up ? These are all viable possibilities and you must have these things flowing freely through your head during the clinical examination as you rule in/rule out your hands-on findings. Remember, just going by a FMS-type screen to drive prescription exercises from what you see on a movement screen is not going to necessarily fix the problem, it could in fact lead one to drive a deeper compensation pattern. You can be sure that Gray Cook’s turbo charged brain is juggling all of these issues (and more !) when he sees a screen impairment, although we are not speaking for him here.
Remember this critical fact. After an injury or a long standing problem, muscles and motor patterns jobs are to stabilize and manage loads (stability and mobility) for adequate and necessary movement. Injuries leave a mark on the system as a whole because adaptation was necessary during the initial healing phase. This usually spills over during the early movement re-introduction phase, particularly if movement is reintroduced too early or too aggressively. Plasticity is the culprit. Just because the injury has come and gone does not mean that new patterns of skill, endurance, strength (S.E.S -our favorite mnemonic), stability and mobility were not subsequently built onto the apparently trivial remnants of the injury. There is nothing trivial if it is abnormal. The forces must, and will, play out somewhere in the body and this is often where pain or injury occurs but it is rarely where the underlying problem lives.
Come back tomorrow, where we will open your mind into the yellow, pink, blue and lime markings on the photo. Are the hammering toes (lime) on the left a clue ? How about the width of the feet (yellow) ? The posturing differences of the 5th toe to the lateral foot border ? What about the static plantar pressure differences from side to side (blue)? Maybe, just maybe, we can bring a logical clinical assumption together and then a few clinical exam methods to confirm or dis-confirm our working diagnostic assumption. See you tomorrow friends !
Shawn and ivo, the gait guys
Here is the case link.......
https://thegaitguys.tumblr.com/post/99409232289/the-standing-on-glass-static-footpedograph?fbclid=IwAR3gd3d81Gwt3ywAB7BcTwXqST2Z_5nmieODzSb8rJQYBcJFhTs6rS_9auA