The partial truth about the Foot Tripod. The HEXApod.
The gait guys have talked about the foot tripod for a very long time. But the truth of the matter is that it is really a HEXApod. HEXA means 6. And when the foot is properly orientated and engaged on the ground, the 5 metatarsal heads and the heel should all be engaged with the ground, truly making it an asymmetrical hexapod. In an ideal scenario, the foot would be most stable if it looked like the strange symmetrical hexapod above with the contact points equally distributed around a center point. But that is not the human foot and this version of a hexapod is far simpler and likely inferior to the foot hexapod when human locomotion is to be attempted. The human foot is engineering marvel when it works properly.
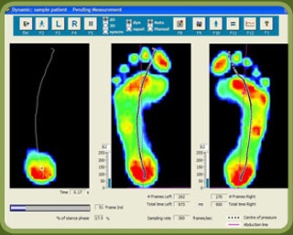
Perhaps the best example of what I mean by the foot being a HEXApod is in the pressure diagram above. In that first picture, on the right of that picture, we see multiple pressure points under the metatarsal heads of the right foot. Minus the missing 1st metatarsal head pressure point (taken over by increased flexor hallucis longus activity represented by increased pressure at the big toe), this pretty much confirms that the foot is not a tripod, rather a hexapod. The theory of the tripod, the 1st and 5th metatarsal heads and the heel, is only crudely accurate and honest. In this picture case, this person has increased lateral foot weight bearing (possibly why the 1st MET head pressure is absent) and possibly represented by pressure under the base of the 5 metatarsal. This is not normal for most people and if this person could get the 1st MET head down, they might even have a HEPTApod foot structure because of the 5th metatarsal base presentation (which sometimes represents peroneal muscle weakness).
Where did we lead you astray after all these years of “tripod” talk ? We have always discussed the foot tripod. We have always discussed the imperative need to keep the limb’s plumb line forces within the area represented by the tripod. If your forces fall more laterally within the tripod, as in this first discussed picture, one is at increased risk of inversion events and the myriad of compensations within the entire body that will occur to prevent that inversion. So again, why the tripod? Well, it is easier to understand and it serves our clients well when it comes to finding active foot arch restoration as seen in this video of ours here. But, the truth of the matter is that all of the metatarsal heads should be on the ground. The 2nd METatarsal is longer, the 3rd a little shorter, and the 4th and 5th even a little short than those. With the 1st MET shorter, these 5 form a kind of parabolic arc if you will. Each metatarsal head still should contact the ground and then each of those metatarsals should be further supported/anchored by their digits (toes) distally. So the foot is actually more truly a HEXAPOD. Take the old TRIPOD theory we have always spoken about and extend a curved line beyond the forefoot bipod points (1st and 5th metatarsals) to incorporate contact points on the 2, 3 and 4th metatarsal heads. These metatarsals help to form the TRANSVERSE arch of the foot. It is this transverse arch that has given us the easily explainable foot TRIPOD because if a line is drawn between just the shorter 1st and 5th metatarsals, we do not see contact of the 2-4 metatarsal heads when we only look for pressure between these two bipod landmarks, but the obvious truth is that the 2-4 metatarsals are just longer and extend to the ground further out beyond this theoretical line drawn between the 1st and 5th MET heads.
So, the foot is a HEXAPOD. Make no mistake about it. It is more stable than a tripod because there are more contact points inside the traditionally discussed foot tripod model. And frankly, the tripod theory is just a lie and just too fundamentally simple, unless you are an American 3 toed woodpecker.
Dr. Shawn Allen, www.doctorallen.co
one of the gait guys