Part 2: “Standing on Glass” Static Foot/Pedograph Assessment
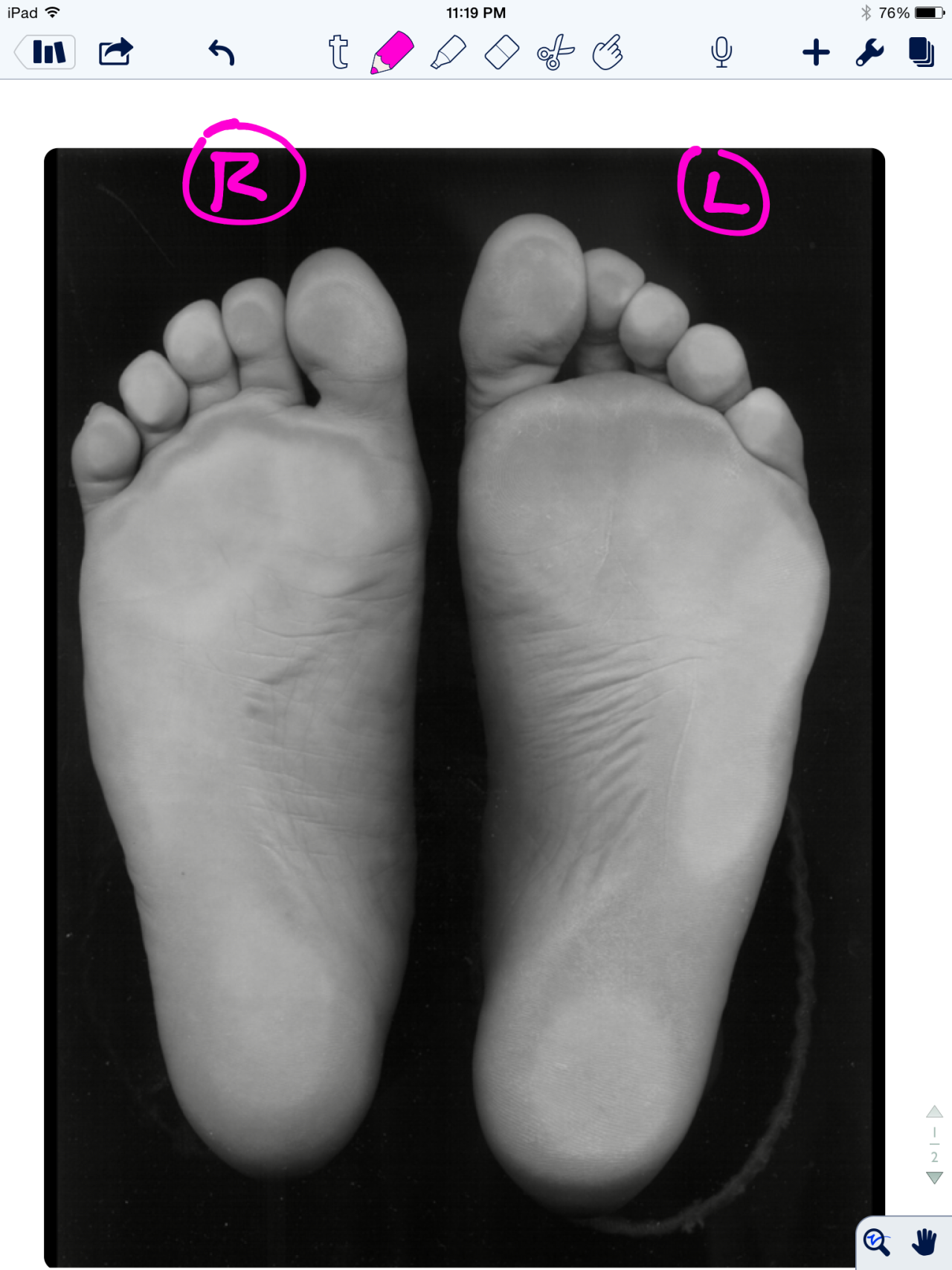
* note (see warning at bottom): This is a static assessment dialogue. One cannot, and must not, make clinical decisions from a static assessment. The right and left sides are indicated by the R and L circled in pink. There are 4 photos here today.
Blue lines: Last time we evaluated possible ideas on the ORANGE lines here, it would be to your advantage to start there.
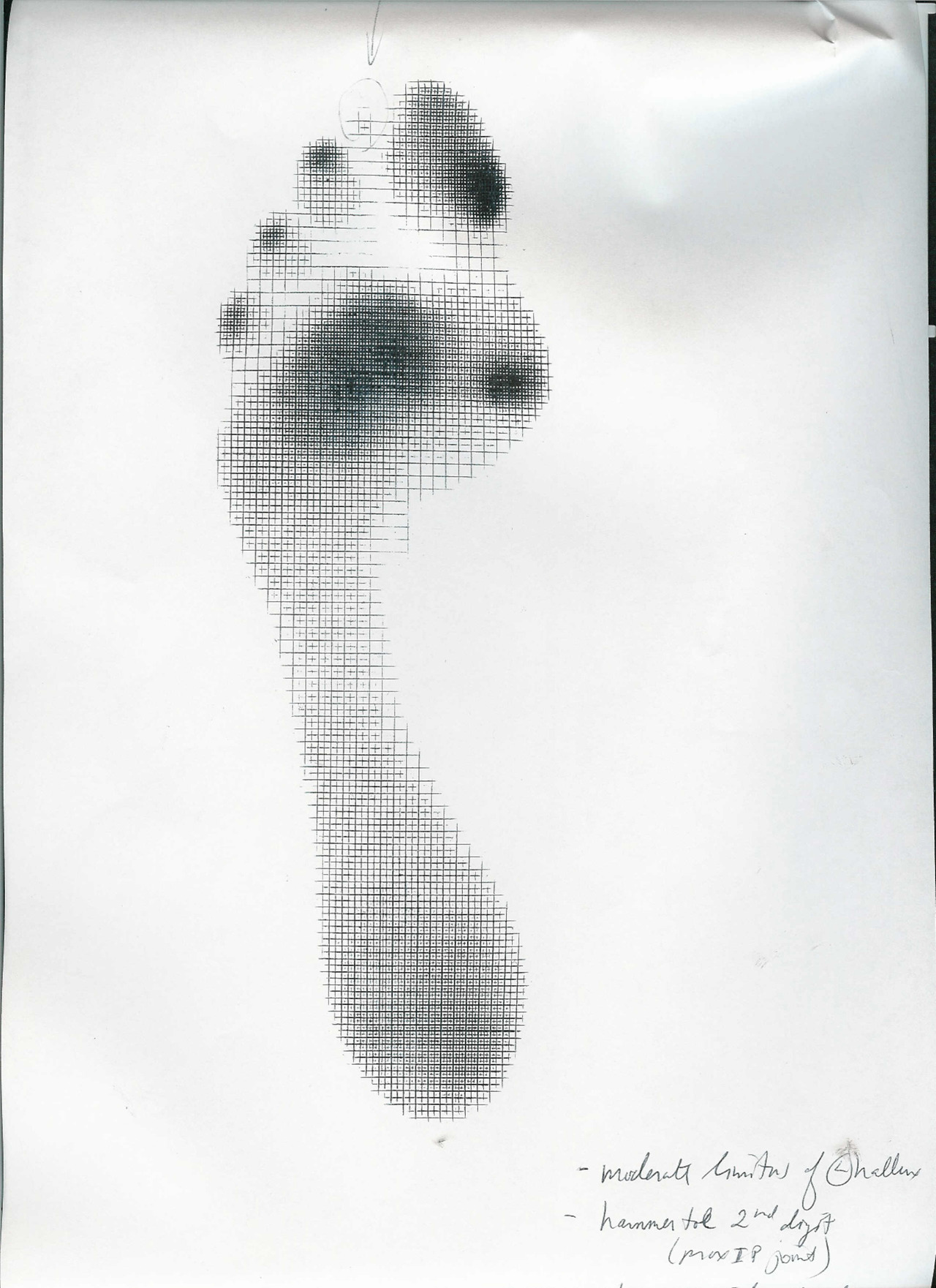
We can see a few noteworthy things here in these photos. We have contrast-adjusted the photo so the pressure areas (BLUE) are more clearly noted. There appears to be more forefoot pressure on the right foot (the right foot is on the readers left), and more rearfoot pressure on the left (not only compare the whiteness factor but look at the displacement of the calcaneal fat pad (pink brackets). There is also noticeably more lateral forefoot pressure on the left. There is also more 3-5 hammering/flexion dominance pressure on the left. The metatarsal fat pad positioning (LIME DOTS represent the distal boundary) is intimately tied in with the proper lumbrical muscle function (link) and migrates forward toward the toes when the flexors/extensors and lumbricals are imbalanced. We can see this fat pad shift here (LIME DOTS). The 3-5 toes are clearly hammering via flexor dominance (LIME ARROWS), this is easily noted by visual absence of the toe shafts, we only see the toe pads. Now if you remember your anatomy, the long flexors of the toes (FDL) come across the foot at an angle (see photo). It is a major function of the lateral head of the Quadratus plantae (LQP) to reorient the pull of those lesser toe flexors to pull more towards the heel rather than on an angle. One can see that in the pressure photos that this muscle may be suspicious of weakness because the toes are crammed together and moving towards the big toe because of the change in FDL pull vector (YELLOW LINES). They are especially crowding out the 2nd toe as one can see, but this can also be from weakness in the big toe, a topic for another time. One can easily see that these component weaknesses have allowed the metatarsal fat pad to migrate forward. All of this, plus the lateral shift weight bearing has widened the forefoot on the left, go ahead, measure it. So, is this person merely weight bearing laterally because they are supinating ? Well, if you read yesterday’s blog post we postulated thoughts on this foot possibly being the pronated one because of its increased heel-toe and heel-ball length. So which is it ? A pronated yet lateral weight bearing foot or a normal foot with more lateral weight bearing because of the local foot weaknesses we just discussed ? Or is it something else ? Is the problem higher up, meaning, are they left lateral weight bearing shift because of a left drifted pelvis from weak glute medius/abdominal obliques ? Only a competent clinical examination will enlighten us.
Is the compensation top-down or bottom up, or both in a feedback cycle trying to find sufficient stability and mobility ? These are all viable possibilities and you must have these things flowing freely through your head during the clinical examination as you rule in/rule out your hands-on findings. Remember, just going by a screen to drive prescription exercises from what you see on the movement screen is not going to necessarily fix the problem, it could in fact lead one to drive a deeper compensation pattern.
Remember this critical fact. After an injury or a long standing problem, muscles and motor patterns jobs are to stabilize and manage loads (stability and mobility) for adequate and necessary movement. Injuries leave a mark on the system as a whole because adaptation was necessary during the initial healing phase. This usually spills over during the early movement re-introduction phase, particularly if movement is reintroduced too early or too aggressively. Plasticity is the culprit. Just because the injury has come and gone does not mean that new patterns of skill, endurance, strength (S.E.S -our favorite mnemonic), stability and mobility were not subsequently built onto the apparently trivial remnants of the injury. There is nothing trivial if it is abnormal. The forces must, and will, play out somewhere in the body and this is often where pain or injury occurs but it is rarely where the underlying problem lives.
Come back tomorrow. We will try to bring this whole thing together, but remember, it will just be a theory for without an exam one cannot prove which issues are true culprits and which are compensations. Remember, what you see is often the compensatory illusion, it is the person moving with the parts that are working and compensating not the parts that are on vacation. See you tomorrow friends !
Shawn and ivo, the gait guys
* note: This is a static assessment dialogue. One cannot, and must not, make clinical decisions from a static assessment. As in all assessments, information is taken in, digested and then MUST be confirmed, denied and/or at the very least, folded into a functional and clinically relevant assessment of the client before the findings are accepted, dismissed and acted upon. As we always say, a gait analysis or static pedograph-type assessment (standing force plate) is never enough to make decisions on treatment to resolve problems and injuries. What is seen and represented on either are the client’s strategies around clinical problems or compensations. Today’s photo and blog post are an exercise in critical clinical thinking to get the juices flowing and to get the observer thinking about the client’s presentation and to help open up the field to questions the observer should be entertaining. The big questions should be, “why do i see this, what could be causing these observances ?”right foot supinated ? or more rear and lateral foot……avoiding pronation ?