“… knowing this will not mistakenly leave one with the interpretation that the joint is suffering restriction, that the joint is merely showing its limitation because of the return shift of the eccentric axis to a less mobile position.” - The Gait Guys
This video is just the kind of stuff that drives us nuts. We do not have a personal problem with the good doctor, he may know (and most likely does know) far more than he is letting on here but is merely simplifying things for some reason. We merely have a problem with the information that is missing that could make this a valuable addition, or omission, to someone’s care. There are times to simplify things, but when we put out a video on the web where the world can see it, we try to be as thorough as possible even if this means that something will come across seemingly overcomplicated. The fact of the matter is that human biomechanics are in fact complicated and simplifying something, when it is just not possible to do so, really doesn’t help anyone. People, and maybe some medical professionals, who do not know better will see this and not see what is missing, importantly so, here.
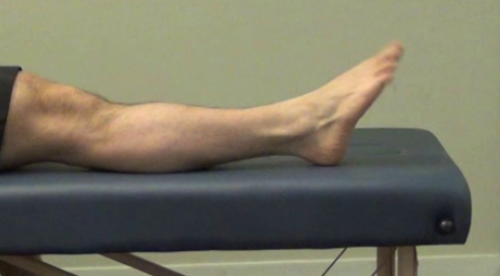
In this video there is no regard to the pre-positioning of the metatarsal to that big toe. This is a very unique joint, it has an eccentric axis that changes with metatarsal plantarflexion and dorsiflexion. This eccentric axis is shifted by the shifting position of the relationship of the metatarsal head with the base of the hallux. Here, at this joint, we have a concave-convex joint interface which with all said joint types, has a roll-glide biomechanical rule. This rule at this joint is unique in that the axis of roll-glide is eccentric meaning that the joint has a shifting axis during the motion of dorsi and plantarflexion. This is dictated and dependent upon the posturing of the sesamoid bones properly beneath the metatarsal head. You can hear more about this premise here, in a video we did a few years ago. It is long, but it is all encompassing. What is important, that which is not noted here, is that with more metatarsal plantarflexion there is opportunistically more dorsiflexion at the joint. (This is precisely the joint range loss that occurs in “turf toe”, hallux limitus.) Thus, in the above video, to properly mobilize the big toe into dorsiflexion, the foot must be taken into full metatarsal plantarflexion (pointing the foot) where greater amounts of joint dorsiflexion will be found (because of the eccentric axis shift) and the joint should be also mobilized in full ankle and metatarsal dorsiflexion, but the therapy giver must know, and be expected to find, that less toe/joint dorsiflexion will ALWAYS be found in this position. Knowing this will not mistakenly leave one with the interpretation that the joint is suffering restriction, that the joint is merely showing its limitation because of the return shift of the eccentric axis to a less mobile position.
* Here is a little experiment you can do to teach yourself this principle. It should also help you to realize the gait cycle.
Sit in a chair, cross one ankle over the opposite knee and see what happens to the joint ranges as you proceed.
- dorsiflex the ankle and big toe. With your muscles only, not your hands, actively pull back the ankle and toe striving to get the most amount possible of dorsiflexion at both joints. You should see that there is some toe dorsiflexion of the big toe.
- now keeping that big toe dorsiflexed as strongly as possible, begin to plantarflex the foot, thus moving the 1st metatarsal into plantarflexion as well. You should note that the relative amount of toe-metatarsal dorsiflexion DRAMATICALLY increases !
- you can also do this passively. This time start at full foot plantarflexion (foot pointed) and passively pull that big toe back into dorsiflexion. A huge range is likely to be found if you have a cleanly functioning foot. Now, try to hold that significant range while you push the ankle into dorsifleixon. At the end of the metatarsal and ankle dorsiflexion range you should feel the big toe start to resist this range you are trying to maintain, the big toe will forcibly start to unwind the dorsiflexion. This is because of the eccentric shift of the joint and tension building in the passive tissues in the bottom of the foot.
- You want, and need, these relationships to occur properly and timely in the gait cycle and there are milliseconds to get it right and that means the entire kinetic chain must be clean of flaws, otherwise compensation will occur. (Note: Blocking or trying to control these issues with a foot bed, shoe type or orthotic can either be helpful therapeutically, or harmful to the chain.)
This is precisely what happens in the gait cycle. During swing phase the foot/ankle is in dorsiflexion to create foot clearance and to prepare the foot tripod for the contact phase with the ground. There is some big toe (hallux) dorsiflexion represented in this swing phase, but it is not a significant amount you likely learned from your own self-demo above, mainly because it is not possible, nor warranted. But, once the foot is on the ground and moving through the late stance phase of gait into heel rise, the ankle is plantarflexing. Thus, the metatarsals are plantarflexing, and this is causing the slide and climb of the metatarsal head up onto the sesamoids. This causes the requisite shift of the axis of the 1st MTP joint (metatarsophalangeal) and affording the greater degree of toe dorsiflexion to occur to allow full foot supination, foot rigidity to sustain propulsive loading and also, never to forget, sufficient hip extension for gluteal propulsion. At this point, the range of the big toe in dorsiflexion is far greater than the dorsiflexion of the joint at ankle dorsiflexion. Impairment of this series of events is what leads to turf toe, hallux limitus as it is called. And when that becomes more permanent, even mobilizing the joint, as seen in the video above or otherwise, is not likely to get you or your client very far in terms of normal gait restoration. And forcing it, won’t made it so either.
Remember this, the kinetic chain exists and functions in both directions. If you are starting with a hip problem that limits hip extension, and thus full range toe off during gait, in time you will lose the end range of the toe-off dorsiflexion range. And any attempts to try and regain it at the foot will fail long term if you do not remedy the hip. "If you don’t use it, you will lose it". So to gain it back actively, sometimes you have to restore all of the functional losses of the entire kinetic chain to get what you are hoping for. And for all you people doing “activation” to the glutes on your athletes, finding you are having to do it over and over and over again…….day after day after day, well … . . we hope you take this blog article to heart and put this thought process into action.
Remember, if you do not have the requisite strength, skill and endurance of the 2 toe extensors and 2 toe flexors as well as sufficient strength of the tibialis anterior (as well as many other components) you are likely to see impairment of this joint. In this environment, do not expect joint mobilizations to offer you anything functionally lasting.
We are not saying that joint mobilizations are useless and unnecessary, not by any means. We are saying that you have to know what you are doing when you do them, so you can get the results you desire or, to realize why you are not getting the results you desire.
Treat your clients with clear biomechanical knowledge and you will get the results you desire. If you go in with limited knowledge, results may speak for themselves.
Gait analysis and understanding movement of the human body is a difficult task. It takes many years to learn the fundamental parameters and then many decades to implement the understanding wisely and with effectiveness. Here at the gait guys, we hope to someday get to this point. We too, are students of gait and gait pathology. It is a journey.
“Once you understand the way broadly, you can see it in all things.” -Miyamoto Musashi
Shawn and Ivo, The Gait Guys