A Wobble in the System: The Gait Changes in Normopressure Hydrocephalus
Can you afford to miss this diagnosis ?
Today, the gait changes in NPH are discussed because as with many neurologic disorders and diseases, subtle gait changes are the first signs. And, in this disorder, you have to catch the gait changes early on in order to give your client the greatest changes of full recovery. Today we couple this blog post with a great video story of a missed case study of NPH.
Normopressure hydrocephalus (NPH) consists of the triad of :
1. gait disturbance
2. urinary incontinence
3. dementia or mental decline
In the most general terms, Normal pressure hydrocephalus (NPH), also referred to as symptomatic hydrocephalus, is caused by a decreased absorption of cerebrospinal fluid (CSF). The resultant increased intracranial pressure can cause ventriculomegaly. In NPH patients, the pressure remains just slightly elevated, but enough to create pressure on the cortical tissues of the brain causing the symptoms above. The vagueness of this problem and its seemingly random symptoms is primarily why this disorder is often missed or misdiagnosed as dementia, Parkinson’s or Alzheimers disorders.
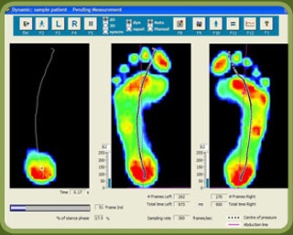
As discussed previously, many early neurological diseases and disorders softly present with early gait changes. And, as in NPH, gait changes may be the earliest symptom of the 3 mentioned earlier. One’s ability to know, observe and recognize abnormal gait patterns coupled with a good historical interview and physical exam can often tease out the earliest manifestation of NPH.
Here is what you need to know about the gait presentation in NPH:
The gait changes are often subtle and progress as NPH progresses because of the changes in the brains ventricular tissues eventually compromising the sensory-motor tracts.
Early gait changes, MILD, may show a cautious gait. Steps length and stride length may be slowed and shortened. The gait may begin to show signs of being deliberate and calculated, less fluid and free. The appearance of unsteadiness or balance challenges may prevail. Once simple environmental obstacles may now present as challenges, things like curbs, stairs, weaving between tables in restaurants or wide open spaces where there is nothing to grasp onto for stability. Weakness and tiredness of the legs may also be part of the complaint, although examination discloses no paresis or ataxia. (Ropper) A walking aid such as a cane may add comfort but often appears to be rarely used.
As the gait changes progress into the more MODERATE to ADVANCED, the walking aids used often progress into quad walkers. Wheelchairs are needed in more difficult places or when fatigue is growing factor. As the gait challenges progress, the careful observer will note a more obvious reduction in step and stride length, a head down posture, less dual tasking engagement during gait execution, slowed walking speed, reduced foot-floor clearance, shuffling gait (keeping the feet more engaged to the ground, this can be a Parkinsonian-type gait mis-read, there will be no tremor or rigidity), searches for stable external cues (reaching for railings, a kind arm or hand, touching walls etc), widening of the feet (broad based stance), and fears of falling backward.
In the most ADVANCED gait impairments, the fear of falling can become too great. There may even be an inability to engage sit-stand-walk motor patterns and the fatigue of the limbs may be too advanced to even stand let along walk. This stage is referred to as Hydrocephalic astasia-abasia (Ropper).
Normopressure Hydrocephalus is a serious issue if left unrecognized and untreated. Here is yet another reason why you must be familiar with this problem:
“Patients with dementia who are confined to a nursing home and may have undiagnosed NPH can possibly become independent again once treated. So far only one study was able to evaluate the prevalence of NPH, both diagnosed and undiagnosed, among residents of assisted-living facilities, showing a prevalence in 9 to 14% of the residents.” - Marmarou
One’s lack of awareness and knowledge, are one’s greatest enemies. If you don’t know something exists, because you’ve never studied or learned it, how can you be aware of it ? If you’re not spending enough time examining a client, you might be unaware of an issue even though you may be knowledgeable about the issue. One must have both awareness and knowledge. One must also be aware that compensations are the way of the body. What you see is not your client’s problem. It is their strategy to cope.
NPH must be diagnosed early on since a delay in reducing the pressure on the cortical tissues can lead to permanency of disease and dysfunction. According to Poca there can be a wide range of successes and failures in symptom remediation, but there is clearly a time dependency on early diagnosis. Thus, clearly recognizing any early gait changes and behaviors prior to advancing incontinence and mental decline is paramount.
Bonus: here is a little bonus tidbit for my fellow neuro gait friends.
Stolze (7) study conclusion: “The gait pattern in normal pressure hydrocephalus is clearly distinguishable from the gait of Parkinson’s disease. As well as the basal ganglia output connections, other pathways and structures most likely in the frontal lobes are responsible for the gait pattern and especially the disturbed dynamic equilibrium in normal pressure hydrocephalus. Hypokinesia and its responsiveness to external cues in both diseases are assumed to be an expression of a disturbed motor planning.”
Dr. Shawn Allen, … one of “the gait guys”
Some of the above was inspired and summarized by this great article, from the Boston Globe.
References:
1. Marmarou, Anthony; Young, Harold F.; Aygok, Gunes A. (1 April 2007). “Estimated incidence of normal-pressure hydrocephalus and shunt outcome in patients residing in assisted-living and extended-care facilities”. Neurosurgical FOCUS 22 (4): 1–8.
2. Ropper, A.H. & Samuels, M.A. (2009). Adams and Victor’s Principles of Neurology (9th edition). New York, NY: McGraw-Hill Medical.
3. Poca, Maria A.; Mataró, Maria; Matarín, Maria Del Mar; Arikan, Fuat; Junqué, Carmen; Sahuquillo, Juan (1 May 2004). “Is the placement of shunts in patients with idiopathic normal pressure hydrocephalus worth the risk? Results of a study based on continuous monitoring of intracranial pressure”. Journal of Neurosurgery 100 (5): 855–866.
4. Am J Phys Med Rehabil. 2008 Jan;87(1):39-45.
Objective assessment of gait in normal-pressure hydrocephalus.
Williams MA1, Thomas G, de Lateur B, Imteyaz H, Rose JG, Shore WS, Kharkar S, Rigamonti D.
5. Clin Neurophysiol. 2000 Sep;111(9):1678-86.
Gait analysis in idiopathic normal pressure hydrocephalus–which parameters respond to the CSF tap test?
Stolze H1, Kuhtz-Buschbeck JP, Drücke H, Jöhnk K, Diercks C, Palmié S, Mehdorn HM, Illert M, Deuschl G.
6.Rev Neurol (Paris). 2001 Nov;157(11 Pt 1):1416-9.
[Postural and locomotor evaluation of normal pressure hydrocephalus: a case report]. Mesure S1, Donnet A, Azulay JP, Pouget J, Grisoli F.
7.J Neurol Neurosurg Psychiatry. 2001 Mar;70(3):289-97.
Comparative analysis of the gait disorder of normal pressure hydrocephalus and Parkinson’s disease.
Stolze H1, Kuhtz-Buschbeck JP, Drücke H, Jöhnk K, Illert M, Deuschl G.