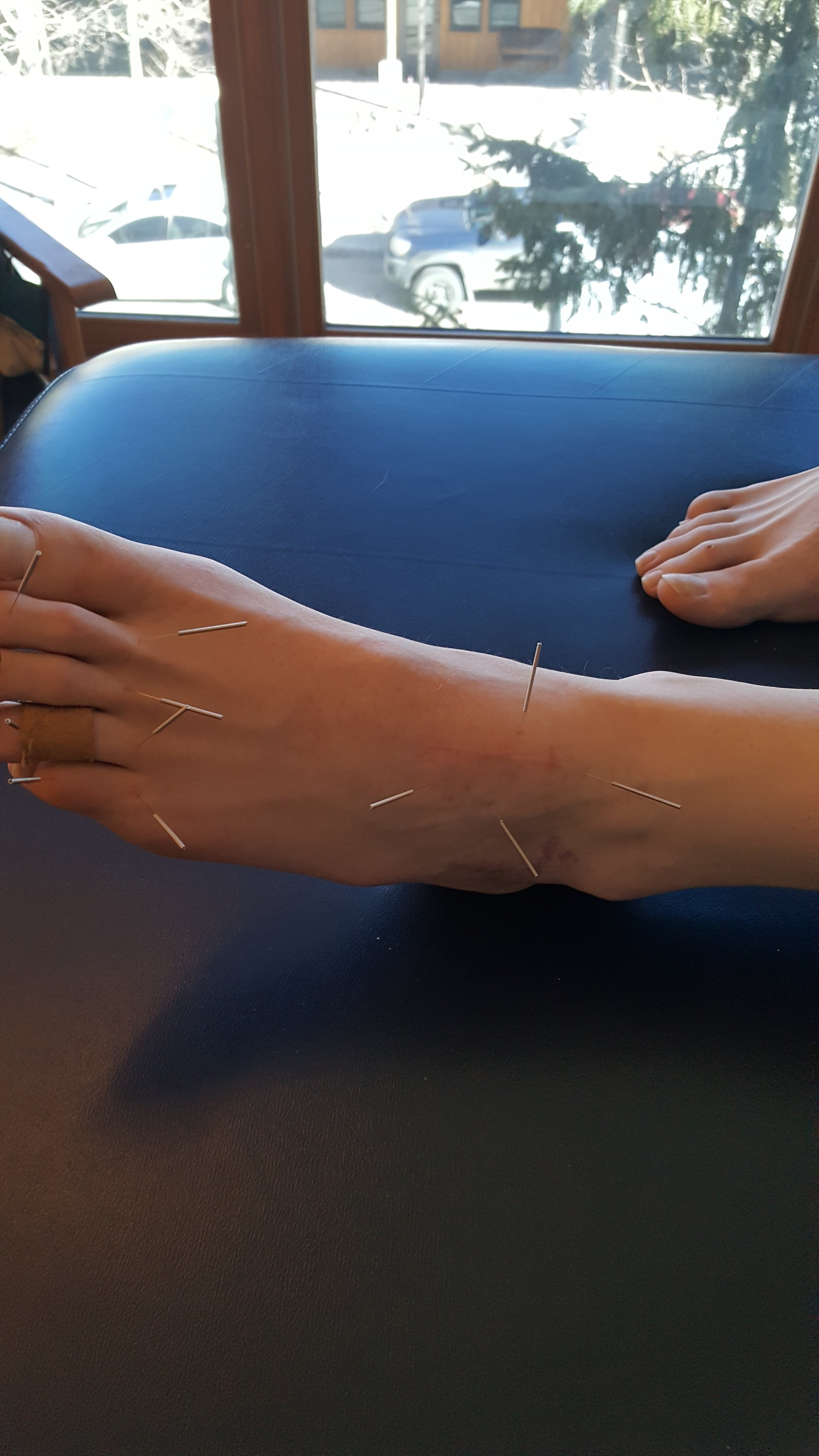
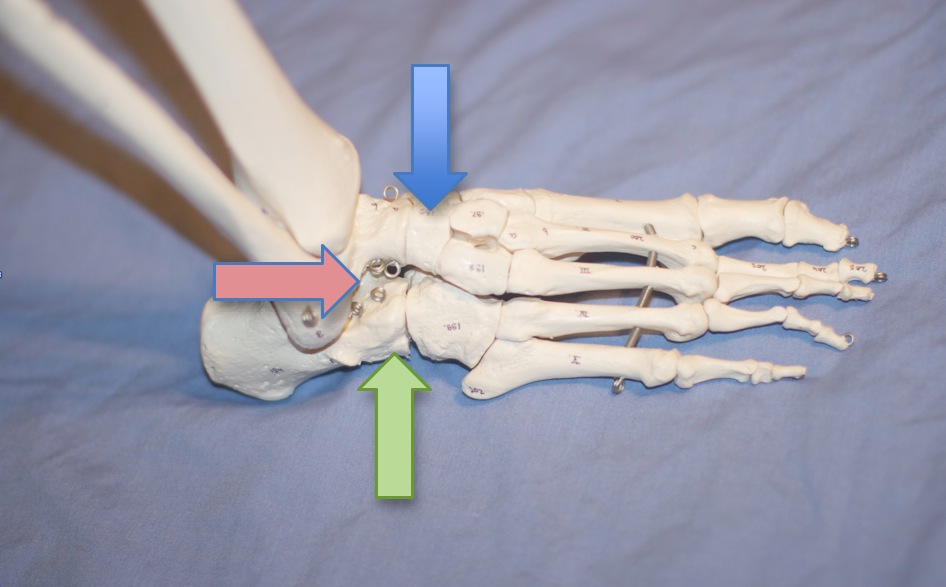
Do you know SQUAT? Have you seen SQUAT? Have patients/clients that LIKE to squat? Seen a foot that looks like this? Can you say REARFOOT VALGUS?
"Significant changes in lower limb kinematics may be observed during bilateral squatting when rearfoot alignment is altered. Shoe pitch alone may significantly reduce peak pronation during squatting in this population, but additional reductions were not observed in the subtalar neutral position. Further research investigating the effects of footwear and the subtalar neutral position in populations with lower limb pathology is required."
So, what does this study tell us?
when rearfoot aliment changes, so do the kinematics (duh)
the surface (tilted into varus or inversion) or shoes (which are medially posted) can make or break the man (or women) when it comes to "peak" pronation (we knew that already; confirmation is always nice)
inverting the rearfoot can change ankle dorsiflexion (read "ankle rocker"); inverting the rearfoot seems to reduce it
inverting the rearfoot can change knee flexion; inverting the rearfoot seems to increase knee flexion
inverting the rearfoot can change hip abduction (and thus knee valgus); reducing it
Learn about the gait kinematics and clinical findings associated with this foot type, along with video clip examples and always entertaining discussion with us tomorrow night on onlinece.com: Biomechanics 308: Focus on the Rear Foot. 5PST, 6MST, 7 CST, 8EST
Power V, Clifford AM. The Effects of Rearfoot Position on Lower Limb Kinematics during Bilateral Squatting in Asymptomatic Individuals with a Pronated Foot Type. J Hum Kinet. 2012 Mar;31:5-15. doi: 10.2478/v10078-012-0001-0. Epub 2012 Apr 3.
#rearfootvalgus #squat #foottype
2012 Mar;31:5-15. doi: 10.2478/v10078-012-0001-0. Epub 2012 Apr 3.
The Effects of Rearfoot Position on Lower Limb Kinematics during Bilateral Squatting in Asymptomatic Individuals with a Pronated Foot Type.
Author information
Abstract
Clinicians frequently assess movement performance during a bilateral squat to observe the biomechanical effects of foot orthotic prescription. However, the effects of rearfoot position on bilateral squat kinematics have not been established objectively to date. This study aims to investigate these effects in a population of healthy adults with a pronated foot type. Ten healthy participants with a pronated foot type bilaterally (defined as a navicular drop >9mm) performed three squats in each of three conditions: barefoot, standing on 10mm shoe pitch platforms and standing on the platforms with foam wedges supporting the rearfoot in subtalar neutral. Kinematic data was recorded using a 3D motion analysis system. Between-conditions changes in peak joint angles attained were analysed. Peak ankle dorsiflexion (p=0.0005) and hip abduction (p=0.024) were significantly reduced, while peak knee varus (p=0.028) and flexion (p=0.0005) were significantly increased during squatting in the subtalar neutral position compared to barefoot. Peak subtalar pronation decreased by 5.33° (SD 4.52°) when squatting on the platforms compared to barefoot (p=0.006), but no additional significant effects were noted in subtalar neutral. Significant changes in lower limb kinematics may be observed during bilateral squatting when rearfoot alignment is altered. Shoe pitch alone may significantly reduce peak pronation during squatting in this population, but additional reductions were not observed in the subtalar neutral position. Further research investigating the effects of footwear and the subtalar neutral position in populations with lower limb pathology is required.