You need toe extension, more than you might think.
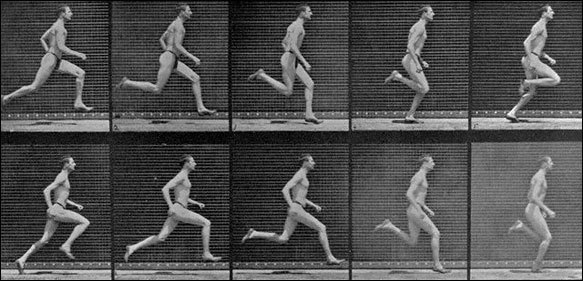
/There is a major difference in these 2 photos.One foot is ready for foot loading, the other has one foot over the starting line, and is going to possibly have the risks related to inappropriate loading.
In clients with one of several possible issues related to poor control of the arch during weight bearing loading, it is not all too uncommon for us to bring to their attention that not only do they NOT utilize toe extension appropriately, and at the right time, they just simply have poor strength and endurance of the toe extensors (we will not be bringing up the complicated orchestration of the long and short toe extensors today, lets just keep it loosely as looking at them as a whole for today).
We know we say it an awful lot, that clients need more toe extension endurance and strength. But more often than not, they need more awareness of how little they are actually using their toe extensors during foot loading. This is why we despise flip flops and foot wear without a back strap on them, the flexors have to dominate to keep the footwear on the foot. And, if you are into your toe flexors, you are definitely not into your toe extensors.
You can easily see in this photo that there is a major difference in the integrity and preparation of the foot arch prior to foot loading in these 2 sample photos. One the toes are up in extension, the other the toes are lazy and neutral. The toe up photo demonstrates well that when the toes are extended, the Windlass mechanism draws the forefoot and rearfoot together and raises the arch. Go ahead, lift your toes, it will happen on you as well (unless your arch is so collapsed that the first metatarsal actually dorsiflexes during toe extension, in this case, you are a whole different management tier). From this arch raised position, the first metatarsal is adequately plantarflexed, this means the joint complexes proximal and distal to the metatarsals are all in the right position to load and cope with loads. In the toe neutral picture, these components are not prepared, the arch is already getting ready to weight bear load from a half-baked position. One cannot expect the foot complex to load well when it is starting from a position of "half way there". One should start the loading of the foot from the starting line, not 3 steps over the line and not 3 steps before the starting line. There is no athletic or mechanical endeavor that does well when we start the challenge too soon or too late, timing is everything.
How you choose to prep your foot for contact loading, and yes, there is some conscious choice here, one is lazy the other is optimal, can determine to a large degree if you or your client is about to fall into the long list of problems related to poorly controlled pronation (too much, too soon, too often, too fast). Any of those bracketed problems lead to improper loading and strains during time under tension.
We will almost always start our clients on our progressing protocol of arch awareness and we will loosely say arch restoration, and attempts at better optimizing the anatomy they have, with toe up awareness. Many clients will have poor awareness of this component issue, on top of poor endurance and frank weakness. The arch is to a great degree build from a lifting mechanical windlass effect, from the extensors and foot dorslflexors, not from the foot flexors. This is one of our primary beefs with the short foot exercise of Janda, there needs to be a toe extensor component in that exercise (search our blog for why the short foot exercise is dead). The short foot exercise is not actually dead, all exercises have some value when placed and performed properly, but the short foot exercise is based off of the toes being down and utilizing the plantar intrinsics to push the arch up and shorten the foot, this is a retrograde motion and it is not how we load the foot, but, it does have value if you understand this and place it into your clients repertoire appropriately. This is also why we have some conceptual problems in stuffing an orthotic under someones arch to "lift it up", ie. slow its fall/pronation. There are times for this, but why not rebuild the proper pathways, patterns and mechanics ?
Teach your clients about toe extension awareness. TEach them that they need to relearn the skill that when the toes drop down to the ground that the arch does NOT have to follow them down, that the client can relearn, "toe up, arch up . . . . . then toes down, but keep the arch up". IT is a mantra in our office, "don't let your arch play follow the leader". Reteach the proper neurologic disassociation between the toes and arch.
Perhaps the first place you should be starting your clients with foot and ankle issues, is regaining awareness of proper toe extension from the moment of toe off, maintaining it through swing, and then keeping it until the forefoot has purchase on the ground again, and not any time sooner than that ! If their toes are coming down prior to foot contact, it is quite likely their arch is following the leader.
So, if your client comes in with any of the following, to name just a few: tibialis posterior tendonitis, plantar fascitis, heel pain, forefoot pain, painful bunions, arch pain, hallux limitus, turf toe, . . . . and the list goes on. Perhaps this will help you get your client to the starting line.
Shawn & Ivo, thegaitguys.com