Lots of links available here with today’s blog post. please make sure to take your time and check out each one (underlined below)
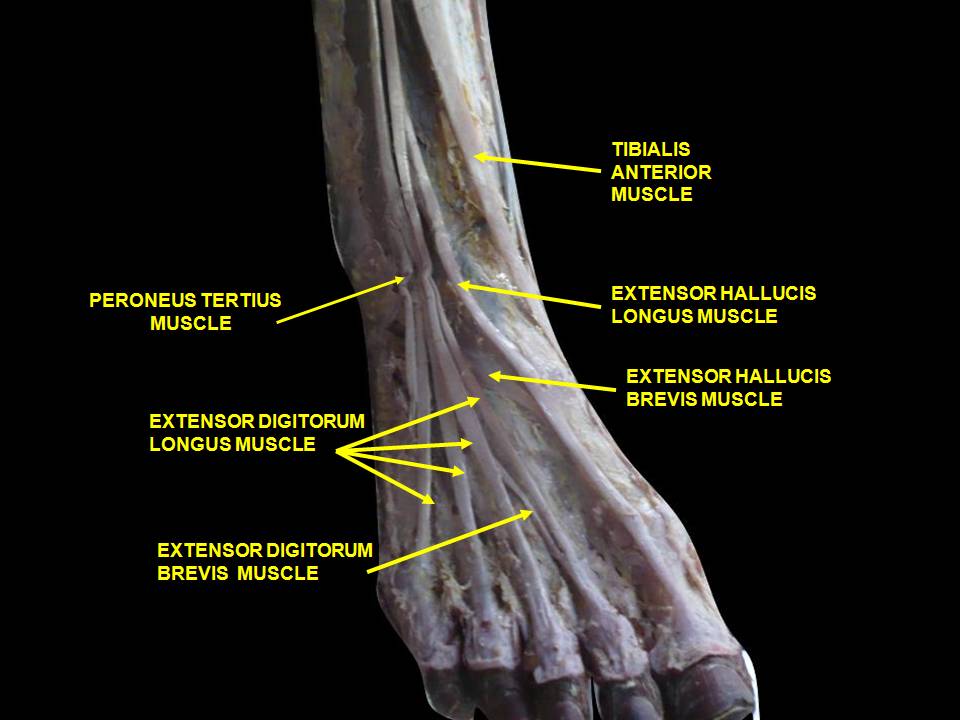
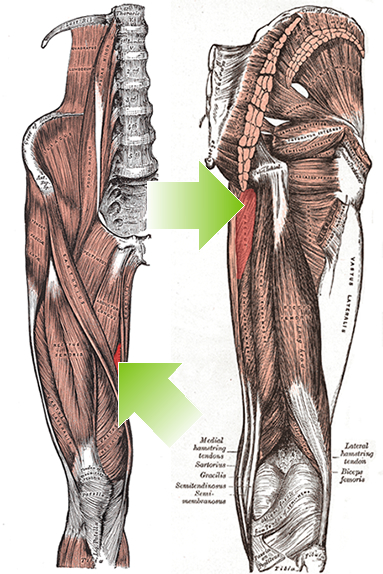
As you remember, the peroneii (3 heads) are on the outside of the lower leg (in a nice, easy to remember order of longus, brevis and tertius, from top to bottom) and help to stabilize the lateral ankle. The peroneus brevis and tertius dorsiflex and evert the foot while the peroneus longus plantarflexes and everts the foot. We discuss the peroneii more in depth here in this post. It then is probably no surprise to you that people with ankle issues, probably have some degree of peroneal dysfunction. Over the years the literature has supported notable peroneal dysfunction following even a single inversion sprain event.
Functional ankle instability (FAI) is defined as “ the subjective feeling of ankle instability or recurrent, symptomatic ankle sprains (or both) due to proprioceptive and neuromuscular deficits."
Arthrogenic muscle inhibition (AMI) is a neurological phenomenon where the muscles crossing a joint become "inhibited”, sometimes due to effusion (swelling) of the joint (as seen here) and that may or may not be the case with the ankle (see here), or it could be due to nociceptive input altering spindle output or possibly higher centers causing the decreased muscle activity.
This paper (see abstract below) merely exemplifies both the peroneals and FAI as well as AMI.
Take home message?
Keep the peroneals strong with lots of balance work!
2009 May;37(5):982-8. doi: 10.1177/0363546508330147. Epub 2009 Mar 6.
Peroneal activation deficits in persons with functional ankle instability.
Palmieri-Smith RM, Hopkins JT, Brown TN.
Source
School of Kinesiology, University of Michigan, 401 Washtenaw Avenue, Ann Arbor, MI 48109, USA. riannp@umich.edu
Abstract
BACKGROUND:
Functional ankle instability (FAI) may be prevalent in as many as 40% of patients after acute lateral ankle sprain. Altered afference resulting from damaged mechanoreceptors after an ankle sprain may lead to reflex inhibition of surrounding joint musculature. This activation deficit, referred to as arthrogenic muscle inhibition (AMI), may be the underlying cause of FAI. Incomplete activation could prevent adequate control of the ankle joint, leading to repeated episodes of instability.
HYPOTHESIS:
Arthrogenic muscle inhibition is present in the peroneal musculature of functionally unstable ankles and is related to dynamic peroneal muscle activity.
RESULTS:
The FAI patients had larger peroneal H:M ratios in their nonpathological ankle (0.399 +/- 0.185) than in their pathological ankle (0.323 +/- 0.161) (P = .036), while no differences were noted between the ankles of the controls (0.442 +/- 0.176 and 0.425 +/- 0.180). The FAI patients also exhibited lower EMG after inversion perturbation in their pathological ankle (1.7 +/- 1.3) than in their uninjured ankle (EMG, 3.3 +/- 3.1) (P < .001), while no differences between legs were noted for controls (P > .05). No significant relationship was found between the peroneal H:M ratio and peroneal EMG (P > .05).
CONCLUSION:
Arthrogenic muscle inhibition is present in the peroneal musculature of persons with FAI but is not related to dynamic muscle activation as measured by peroneal EMG amplitude. Reversing AMI may not assist in protecting the ankle from further episodes of instability; however dynamic muscle activation (as measured by peroneal EMG amplitude) should be restored to maximize ankle stabilization. Dynamic peroneal activity is impaired in functionally unstable ankles, which may contribute to recurrent joint instability and may leave the ankle vulnerable to injurious loads.