Pain on the outside of one leg, inside of the other.
Whenever you see this pattern of discomfort, compensation is almost always at play and it is your job to sort it out.
This patient presents with with right sided discomfort lateral aspect of the right fibula and in the left calf medially. Pain does not interfere with sleep. He is a side sleeper 6 to 8 hours. His shoulders can become numb; left shoulder bothers him more than right.
PAST HISTORY: L shoulder surgery, rotator cuff with residual adhesive capsulitis.
GAIT AND CLINICAL EVALUATION: see video. reveals an increased foot progression angle on the right side. Diminished arm swing from the right side. A definite body lean to the right upon weight bearing at midstance on that side.
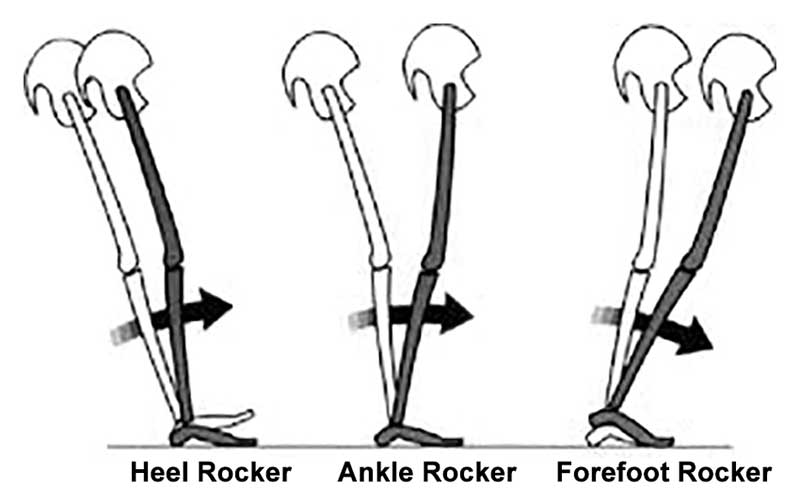
He has external tibial torsion bi-lat., right greater than left with a right short leg which appears to be at least partially femoral. Bi-lat. femoral retrotorsion is present. Internal rotation approx. 4 to 6 degrees on each side. He has an uncompensated forefoot varus on the right hand side, partially compensated on the left. In standing, he pronates more on the left side through the midfoot. Ankle dorsiflexion is 5 degrees on each side.
trigger points in the peroneus longus, gastroc (medial) and soles.
Weak long toe extensors and short toe flexors; weak toe abductors.
pathomechanics in the talk crural articulation b/l, superior tip/fib articulation on the right, SI joints b/l
WHAT WE THINK:
1. This patient has a leg length discrepancy right sided which is affecting his walking mechanics. He supinates this extremity as can be seen on video, especially at terminal stance/pre swing (ie toe off), in an attempt to lengthen it; as a result, he has peroneal tendonitis on the right (peroneus is a plantar flexor supinator and dorsiflexor/supinator; see post here). The left medial gastroc is tender most likely due to trying to attenuate the midfoot pronation on the left (as it fires in an attempt to invert the calcaneus and create more supination). see here for gastroc info
2. Left shoulder: Frozen shoulder/injury may be playing into this as well as it is altering arm swing.
WHAT WE DID INITIALLY (key in mind, there is ALWAYS MORE we can do):
- build intrinsic strength in his foot in attempt to work on getting the first ray down to the ground; EHB, the lift/spread/reach exercises to perform.
- address the leg length discrepancy with a 3 mm sole lift
- address pathomechanics with mobilization and manipulation.
- improve proprioception: one leg balancing work
- needled the peroneus longus brevis as well as medial gastroc and soles.
- follow up in 1 week to 10 days.
Pretty straight forward, eh? Look for this pattern in your clients and patients