A video case of a gait impairment. Chronic dorsal foot pain.
This client came to see us recently. They had a current (2 year) history of dorsal foot achey/burning pain and anterior ankle pain, right greater than left. They had been just about everywhere for these complaints and were pretty much resolved that it was not fixable. They also had a chronic history of anterior shin splints.
This is a pretty simple case. It is missed alot of the time. The reason it is missed is because nothing much shows up on examination. However, we used some tricks to bring out their symptoms. There are also some subtle hints on the gait video above but when you cannot pair what you see with what you find on a clinical exam the issues can get lost in the mix, as they did in this case. This is thus a case based much on clinical experience. We have seen this before. A great clinician (who’s name we have forgotten) used to have a quote that went something like this:
It is only after you have seen the beast once before that it will serve you well to be able to recognize it the next time. Having never seen the beast previously will leave you with a terrible bloody battle on how to slay it the first go-round.“
ln this video above you should basically see 2 things:
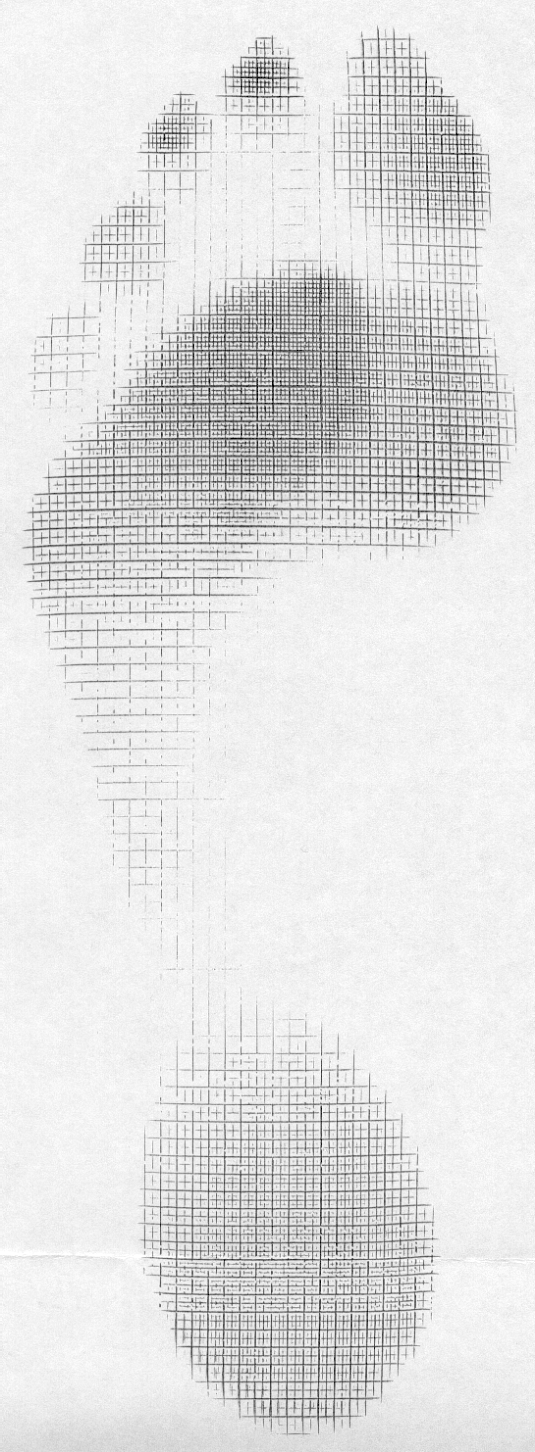
1. the easy one to see: the right foot immediately after toe off does not come forward sagitally rather it spins out into abduction in the swing phase to prepare for the next heel strike.
2. the harder one to see: both feet pronate immediately in the rear and mid foot excessively.
This patient has some limitations in normal ankle rocker. More simply put, they cannot get enough adequate tibial progression forward into dorsiflexion over the talar dome. The squat test was really the only positive movement assessment that was confirmatory. As they squatted the ankle met early dorsiflexion restriction and thus the foot had no choice but to pronate early and heavily thus collapsing medially and drawing the knees in medially. Normally the arch should remain unaffected and the tibia should merely pivot cleanly and effortlessly over the talus allowing the knees to come purely forward. Not in this case.
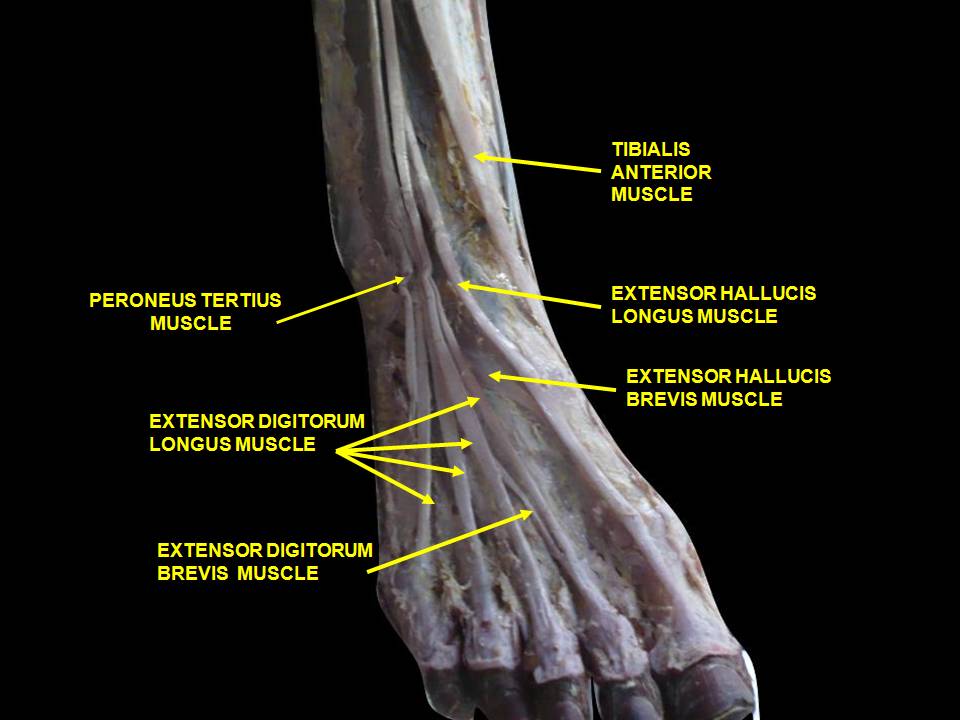
So, we have a client that has impaired sagittal mechanics. They cannot move through ankle rocker effectively and thus they cannot pronate in a timely manner. As the right foot leaves the ground at toe off they need to have sufficient ankle dorsiflexion to carry the foot cleanly forward to prepare for heel strike (this looks pretty good on the left in the video) but the right side is met with ankle range loss. If they did not circumduct the right foot like you see here they would drag their toes on the ground and likely trip. So, foot abduction is the strategy to avoid this issue. However, when you circumduct the foot you begin to lose the strength and endurance of the toe extensors and tibialis anterior.
There is it, we just gave it away. Your question all along should have been, "but what about the dorsal foot and anterior ankle pain and chronic shin splint history?”.
After our gait assessment and history we had a strong hunch. We did our clinical exam which was unremarkable, mostly. But we saw some things that might correlate with our hunches. So, we put the client on our Total Gym at 45 degree incline to do some partially weight bearing squats. Simple stuff. But, we put the feet in a challenged position. We had them hold a neutral foot position on the platform (zero degree progression ankle), the foot was not allowed to spin. We told them they had to keep the toes up at all times and directed them to not let the arch drop or heel spin (these are all compensations to get around impaired ankle rocker in gait, and we see them in her gait video). It seemed simple to them so they began to squat repeatedly, slowly with good form. At about 2 minutes into the movement challenge there began some burning and achey pain reproduction at the dorsal foot from the toes to the anterior ankle. Then it started up their shins. The knees began to hurt. Their toes began to lose their earlier extension/lift. They then started to avoid the depth of the initial first squats so we made them aware and insisted they challenge the initial ranges. After about another 30 seconds the anterior ankle pain began. Our exam was pretty much done. We went back into the room, their pain had stopped. On the exam table it was clear that they now had more toe extension and ankle dorsiflexion range but had no strength in this new range. You see, they initially tested strong in these ranges, but they were strong only in the limited range available to them. On our exam we felt that the ranges were a bit meager, but for some people that is just their anatomy. But we had to be sure, so we gently drove some of those old lost ranges and our examination was concluded.
So, it turns out that this patient had enough weakness in the tibialis anterior and long toe extensors (EDL) sufficient enough to lose ankle rocker ranges over time. When you lose ankle rocker range you meet resistance early. This means you will begin pronation in the foot earlier than normal and begin one or several compensations:
- arch collapse
- heel abduction twist
- increased foot splay (progression angle)
- external limb rotation (paired usu. with #3)
- foot circumduction
- medial knee collapse
- just to name a few…… knee hyperextension etc
Chronic fatiguing and weakness of the toe extensors and tibialis anterior are frequent findings in many people. Sometimes they are subtle and you have to tease them out.
Now, remember the initial pain quality ? Achey burning pain. Now, lets review last weeks pain posts.
Remember the Krebs cycle? How about glycolysis? What was one of the end products of glycolysis? Lactic acid. Your ability to recycle it and make it into oxaloacetic acid and stuff it back into the Krebs cycle determines your aerobic capacity. When lactic acid builds up, we get muscular inefficiency due to the drop in pH (initially this helps, but too much of a good thing creates a problem), The result? Burning pain. Burning pain is the burn of glycolysis, or muscular overuse.
Aching/ throbbing pain is that deep, boring pain, like a toothache in a bone. It is the pain of the mesoderm, or what is often called sclerotogenous pain. Aching/Throbbing pain is the pain of connective tissue dysfunction (remember that connective tissue is bone, cartilage and collagenous structures like ligaments and tendons). Throbbing pain can sometimes be vascular in origin, as the connective tissue elements of the vessels (the tunica adventitia to be exact) is stretched (which contains a perineural plexus; think about the pain of a migraine headache).
This client had fatigue weakness. This is a physiologic energy production issue. Thus the BURNING pain in the toe extensor muscles. They also had the chronic achey pain of sclerotogenous referral from connective (mesoderm) tissue challenges.
See how this all comes together ?! Putting the pieces together is not hard once you know what the pieces are supposed to do and what their limitations are. Then you have to listen to them and hear what they are telling you.
This was a case that did not have to go on for 2+ years. This client did not need to suffer and become a shoe and orthotic obsessed fanatic (searching for answers on their own). Their body was screaming for someone to just listen and look at its communications.
We started them with our famous Shuffle Walks to drive toe extension, ankle rocker/tibialis anterior strength and then showed them how to use more of both during normal gait. As with most of the cases like this. We will let them go for 2-3 weeks to improve these SKILL and ENDURANCE components of the movement pattern. We bet this one will take 2-3 visits to resolve. As endurance builds and then as STRENGTH (the last component) builds they will own the changes and be pain free. And then return to then normal shoe shopping habits like the rest of the world.
We are The Gait Guys……..saving humanity from the scourge of gait related pain, one lovely person at a time.
Shawn and Ivo