Calf Size Matters
/Calf size matters. Truly, and here is why.
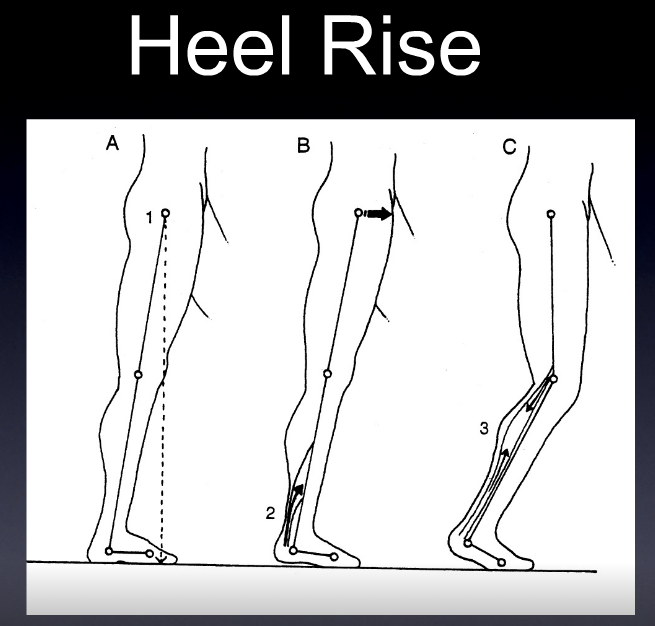
The Achilles tendon (AT) moment arm transforms triceps surae muscle forces into a moment about the ankle which is critical for functional activities like walking and running. The achilles tendon moment arm changes continuously during walking. It changes as movement occurs and as the triceps surae contracts. But, it also changes as the muscle grows in size, or shrinks. This has relevance to exercise, strengthening, and atrophy of the calf compartment. When the muscle contracts, its cross sectional area changes, and this can change the pull angle on the achilles. One might think of the achilles tendon as being "tented" away from the tibia slightly, and one can feel this on their own foot when palpating the soft tissue space between the tendon and the tibia on plantarflexion even when sitting. Better yet, sit down, your foot on the ground. Now, palpate the soft tissue space between the achilles and tibia. Now raise your heel, thus forefoot loading. You will feel the space gap open, the moment arm has increased because of this, thus changing its moment arm. On dorsiflexion the moment arm shortens, on plantarflexion it lengthens. Sure, this does not create a monstrous line of pull change, but by the time we get down to the pivot point at the ankle mortise, a small change in moment arm can translate to significant changes in torque and force production. This is why a foot that does not supinate in time for heel off, or supinate sufficiently, meaning the rear foot isn't inverted optimally, means that the ankle mortise (talus position) might change/shorten that moment arm. This is not efficient mechanics. Want to jump higher ? You have to get that excessive pronation in ankle dorsiflexion under control and convert it to supination, and rearfoot inversion. Jumping from a collapsed foot tripod is a power leak and you will not optimize the triceps surae-achilles complex and their lever arm. This also goes for toe off in walking and especially running, particularly sprinting where you are up on that forefoot. Said another way, when the arch is more collapsed and the talus is thus more plantarflexed the moment arm is sorter for the achilles. Strength, power, torque all suffer. One does not want to engage heel rise and calf contraction from this ineffective position of pronation taken too far, or heel rise while still pronated. This can also put undue load, and angle of pull, through the achilles. Meaning, the linear pull one desires through the achilles, can be through a calcaneal insertion that is not oriented optimally. One might postulate, rightly so we believe, that the lateral bundles/fascicles of the achilles tendon might see more loading than the medial. At the very least, we might postulate that the medial and lateral achilles tensile loads are offset and unequal. This could create problems over time, meaning changes in tendon morphology.
In the below Rasske & Franz article, they posit that aging negatively effects the architecturally complex AT moment arm during walking, which thereby contributes to well-documented reductions in ankle moment generation during push-off. They looked at the "AT moment arms of young (23.9 ± 4.3 years) and older (69.9 ± 2.6 years) adults during walking, their dependence on triceps surae muscle loading, and their association with ankle moment generation during push-off. Older adults walked with 11% smaller AT moment arms and 11% smaller peak ankle moments during push-off than young adults. Moreover, as hypothesized, these unfavourable changes were significantly and positively correlated (r2 = 0.38, p < 0.01). More surprisingly, aging attenuated load-dependent increases in the AT moment arm (i.e., those between heel-strike and push-off at the same ankle angle); only young adults exhibited a significant increase in their AT moment arm due to triceps surae muscle-loading. Age-associated reductions in triceps surae volume or activation, and thus muscle bulging during force generation, may compromise the mechanical advantage of the AT during the critical push-off phase of walking in older adults. Thus, strategies to restore and/or improve locomotor performance in our aging population should consider these functionally important changes in musculoskeletal behavior."
Great article spawning deeper thoughts, here at The Gait Guys blog.
More to come on this most likely.
Aging effects on the Achilles tendon moment arm during walking. Kristen Rasske, Jason R.Franz
Journal of Biomechanics
Volume 77, 22 August 2018, Pages 34-39
Photo credit: Image by Huei-Ming Chai, National Taiwan University School of Physical Therapy as found on www.runsmartproject.com