Do you know your Torsions? If so, then you here is what you need to know about twisted people...
/Are you twisted? Are your patients/clients twisted? You know about tibial torsions from yesterday but do you know about femoral torsions?
To go along with yesterdays post, here is some more info on femoral torsions. If you missed it, click here
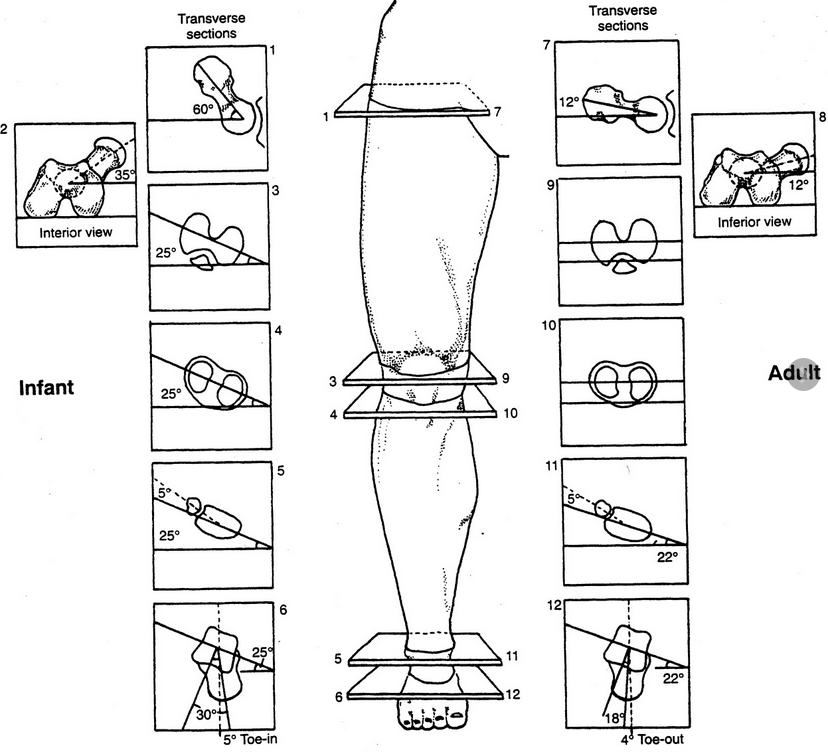
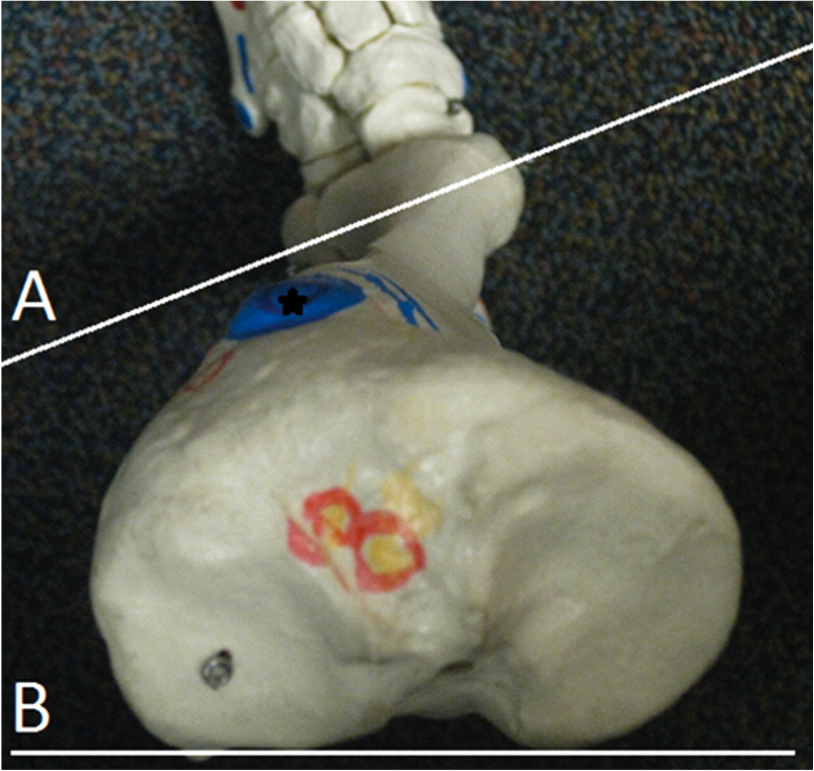
The degree of version is the angle between an imaginary line drawn through the condyles of the femur and an imaginary line drawn through the head and neck of the femur. This is often referred to as the femoral neck angle or FNA.
IMAGE SOURCE: Michael T Cibulka; Determination and Significance of Femoral Neck Anteversion, Physical Therapy, Volume 84, Issue 6, 1 June 2004, Pages 550–558, https://doi.org/10.1093/ptj/84.6.550
Beginning about the 3rd month of embryological development (Lanz and Mayet 1953) the femoral neck angle reaches 60 degrees and decreases, with growth, to about 40 degrees (with an average of 30-60 degrees) at birth. It then decreases 25-30 degrees by adulthood to 8-20 degrees with males being at the lower and females at the upper end of the range.
The FNA angle, therefore, diminishes about 1.5 degrees a year until about 15 years of age. Femoral neck anteversion angle is typically symmetrical from the left side to the right side.
What causes torsion in the first place? By the sixth month in utero, the lumbar spine and hips of the fetus are fully flexed, so perhaps it is positional. Other sources say it coincides with the degree of osteogenesis. There is a growing consensus that muscular forces are responsible, particularly the iliopsoas or possibly the medial and lateral hip rotators.
Additional changes can occur after birth, particularly with sitting postures. “W” sitting or “cross legged” sitting have been associated with altering the available range of motion and thus the FNA, with the range increased in the direction the hip was held in; W sitting causing increased internal rotation and antetorsion and cross legged causing external rotation and retro torsion.
image source: T Michaud, with permission
As discussed previously, there are at least 3 reasons we need to understand torsions and versions, They can alter the progression angle of gait, they usually affect the available ranges of motion of the limb and they can alter the coronal plane orientation of the limb.
fermoral torsions often alter the progression angle of gait. In femoral antetorsion torsion, the knees often face inward, resulting in an intoed gait and a decreased progression angle of the foot. This can be differentiated from internal tibial torsion (ITT) by looking at the tibia and studying the position of the tibial tuberosity with respect to the foot, particularly the 2nd metatarsal. In ITT, the foot points inward while the tibial tuberosity points straight ahead. In an individual with no torsion, the tibial tuberosity lines up with the 2nd metatarsal. If the tibial tuerosity and 2nd met are lined up, and the knees still point inward, the individual probably has femoral ante torsion. Remember that a decreased progression angle is often associated with a decreased step width whereas an increased angle is often associated with an increased step width.
Femoral torsions affect available ranges of motion of the limb. We remember that the thigh leg needs to internally rotate the requisite 4-6 degrees from initial contact to midstance (most folks have 40 degrees) If it is already fully internally rotated (as it may be with femoral retro torsion), that range of motion must be created or compensated for elsewhere. This, much like internal tibial torsion, can result in external rotation of the affected lower limb to create the range of motion needed.
Femoral retro torsion results in less internal rotation of the limb, and increased external rotation.
Femoral ante torsion results in less external rotation of the limb, and increased internal rotation.
3. femoral torsions usually do not effect the coronal plane orientation of the lower limb, since the “spin” is in the transverse or horizontal plane.
The take home message here about femoral torsions is that no matter what the cause:
FNA values that exist one to two standard deviations outside the range are considered “torsions”
Decreased values (ie, less than 8 degrees) are called “retro torsion” and increased values (greater than 20 degrees) are called “ante torsion”
Retro torsion causes a limitation of available internal rotation of the hip and an increase in external rotation
Ante torsion causes an increase in available internal rotation of the hip and decrease in external rotation
Femoral ante torsion will be perpetuated by “W” sitting (sitting on knees with the feet outside the thighs, promoting internal rotation of the femur)
Femoral antetorsion will be perpetuated by sitting cross legged, which forces the thigh into external rotation.
Michael T Cibulka; Determination and Significance of Femoral Neck Anteversion, Physical Therapy, Volume 84, Issue 6, 1 June 2004, Pages 550–558, https://doi.org/10.1093/ptj/84.6.550
http://www.clinicalgaitanalysis.com/faq/torsion.html
Souza AD, Ankolekar VH, Padmashali S, Das A, Souza A, Hosapatna M. Femoral Neck Anteversion and Neck Shaft Angles: Determination and their Clinical Implications in Fetuses of Different Gestational Ages. Malays Orthop J. 2015;9(2):33-36.