Walking and Running Require Greater Effort from the Ankle than the Knee Extensor Muscles.
/Attached is an older video from a few years back , it is very similar in execution to the heel-rise ball squeeze exercise which is the precursor to this more functional engagement as shown in this video today.
The important premise is that you have to have command of the entire posterior compartment if you are to get safe, effective, efficient and adequate ankle plantarflexion. As we have discussed many times, if you do not have the requisite skills as shown in this video you are in trouble and ankle sprains and other functional pathologies are not unlikely to visit you. Additionally, without requisite posterior compartment endurance and an ability to engage what I like to refer to as "top end" strength in the heel rise is an asymmetrial loading issue and can lead to compensatory adaptations up the kinetic chain. Make no mistake, the load will go somewhere, and thus the work will be done somewhere. In this video you should be able to clearly see and understand that one must be able to achieve top end posturing and have command of lateral and medial forefoot loading responses and challenges if clean forward function and power is to be achieved, and injuries from extremes of motion medially and laterally are to be avoided. Furthermore, as eluded to here and in several of our podcasts (and in the study included below), an inability to achieve top end posturing will lead to changes in forefoot loading, may spill over into endurance challenges prematurely in the posterior mechanism, and create changes in the timing of the gait cycle (things like premature or delayed heel rise, premature or delayed forefoot loading, recruitment of other components of the posterior chain just to name a few). This parsing and sharing of loads and responsibilities is laid out in the Kulmala study referenced today. The study could be extrapolated to say, I believe, that particularly in sprinting, a failure to achieve top end heel rise through effective posterior mechanism contraction, will change the load sharing between the posterior compartment and the quadriceps. After all, if the calf is weak, the ankle is not in as much plantarflexion, this could mean more knee flexion and thus raise demands on the quadriceps, logically changing knee mechanics. This is exactly why we spend so much time at every patient visit looking for full range of motion at the joints and then determine the skill, endurance and strength of the associated muscles in supporting that range. Then, of course, comparing this function to the opposite limb. Symmetry is not everything, but it is definitely a major factor in safe efficient and injury free locomotion.
* Please give great thought to the part in the video where I discuss the drop phase in jumping. All too often we at looking for the propulsive mechanics and forget that a failure there will also be represented during the adaptive phase. Ankle sprains rarely occur from propulsive pushing off, they occur from a failure to properly reacquaint the foot to the ground on the following step.
-Dr. Shawn Allen, one of the gait guys.
In this study the authors noted:
"During walking, the relative effort of the ankle extensors was almost two times greater compared with the knee extensors. Changing walking to running decreased the difference in the relative effort between the extensor muscle groups, but still, the ankle extensors operated at a 25% greater level than the knee extensors. At top speed sprinting, the ankle extensors reached their maximum operating level, whereas the knee extensors still worked well below their limits, showing a 25% lower relative effort compared with the ankle extensors."
And concluded that:
"Regardless of the mode of locomotion, humans operate at a much greater relative effort at the ankle than knee extensor muscles. As a consequence, the great demand on ankle extensors may be a key biomechanical factor limiting our locomotor ability and influencing the way we locomote and adapt to accommodate compromised neuromuscular system function."
Med Sci Sports Exerc. 2016 Nov;48(11):2181-2189. Walking and Running Require Greater Effort from the Ankle than the Knee Extensor Muscles. Kulmala JP1, Korhonen MT, Ruggiero L, Kuitunen S, Suominen H, Heinonen A, Mikkola A, Avela J.
https://www.ncbi.nlm.nih.gov/pubmed/27327033
https://youtu.be/8T9UzOaYxmo
the gait guys
#gait, #gaitproblems, #thegaitguys, #gaitanalysis, #heelrise, #calfstrength, #toeoff, #forefootloading, #metatarsalgia, #inversionsprain


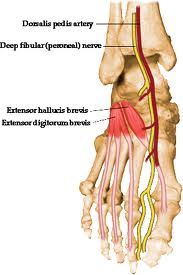 Did you know that the EHB (extensor hallucis brevis) the topic of today’s video tutorial, originates off of the forepart of the medial aspect of calcaneus & lateral talocalcaneal ligament. It is just above the bulk origin of the EDB (extensor digitorum brevis). It is frequently torn/strained in ankle inversion sprains and frequently goes undiagnosed. It can be torn/avulsed from the bone if the inversion sprain is focused below the lateral ankle joint. This occurs mostly when the foot is more plantarflexed before the inversion event. A foot cannot afford to have an impaired big toe ! Don’t miss this one !
Did you know that the EHB (extensor hallucis brevis) the topic of today’s video tutorial, originates off of the forepart of the medial aspect of calcaneus & lateral talocalcaneal ligament. It is just above the bulk origin of the EDB (extensor digitorum brevis). It is frequently torn/strained in ankle inversion sprains and frequently goes undiagnosed. It can be torn/avulsed from the bone if the inversion sprain is focused below the lateral ankle joint. This occurs mostly when the foot is more plantarflexed before the inversion event. A foot cannot afford to have an impaired big toe ! Don’t miss this one !














