Recent trails found in Tanzania suggest fully upright walking began 3.7 million years ago.
The footprints they found suggest that the fully upright gait of present day humans existed about 2 million years prior than previously thought !
“The shape of the human foot is probably one of the most obvious differences between us and our nearest living relatives, the great apes. The difference in foot function is thought to be linked to the fact that humans spend all of their time on the ground, but there has been a lot of debate as to when in the fossil record these changes occurred. Our work shows that there is considerably more functional overlap than previously expected,” Bill Sellers, of the University of Manchester’s Faculty of Life Sciences, said in a University of Liverpool news release.
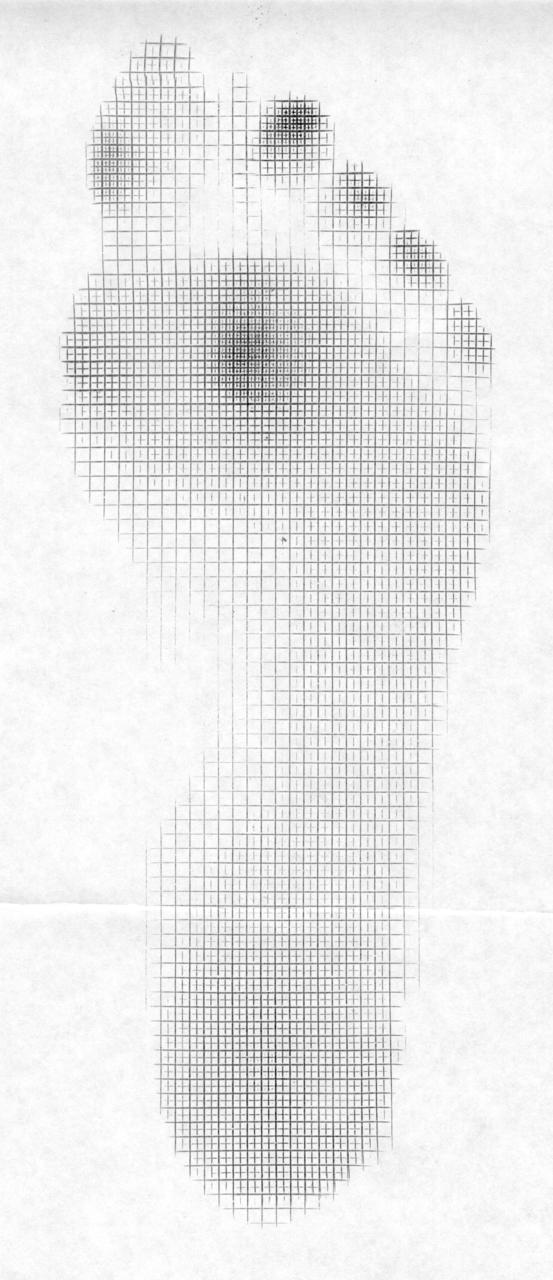
Known as the Laetoli trail, the 11 individual footprints found in Tanzania are the earliest known footprints made by human ancestors. The prints reveal features of a gait with more similarities to the way modern humans walk than the bipedal walking of chimpanzees, orangutans and gorillas.
The study found that instead of the crouched walking posture with mid foot push off of present day apes, the researchers found that these new found foot impressions categorize a bipedal upright walk driven off the front of the foot and largely the big toe highly representative of the human gait of today.
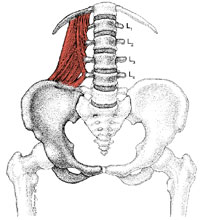
This study suggested that Australopithecus afarensis had a much different build than that of modern day humans. Their build had a long torso and short legs. A reverse of modern man’s physique. Thus, this studies researchers proposed that this species could only ambulate bipedally for short distances.
_______________________________
Click on the title link at the top for the link to the copywrited article. Excerpts quoted from the article.
So, if you are a believer in evolution (or, have been watching “Ancient Aliens”, the Docu-series on The History Channel {wry humor}) ……. then this is worthy of longer term memory.
Q. Why is this article here and why do we deem it important to share with you ?
A. Because history is full of clues. To be good in this field of gait and motion, we feel that you should have a decent foundation in anatomy, neurology and physiology, store facts, keep an open mind, study the research (both old and new), do not discount historical information merely because it is old, and consider all options and possibilities so that knowledge can follow from more current experiences).
(Fact: such memory items are encoded by your hippocampus, entorhinal cortex, and perirhinal cortex, but consolidated and stored mostly (we think) in your temporal cortex.
Tidbit on memory:
In gait, Procedural memory refers to movements of the body, such as how exactly to use use a phone, walk or ride a bicycle. This type of memory is encoded and probably stored by the cerebellum and the striatum.
have a good week everyone…….. The Gait Aliens……. Shawn and Ivo