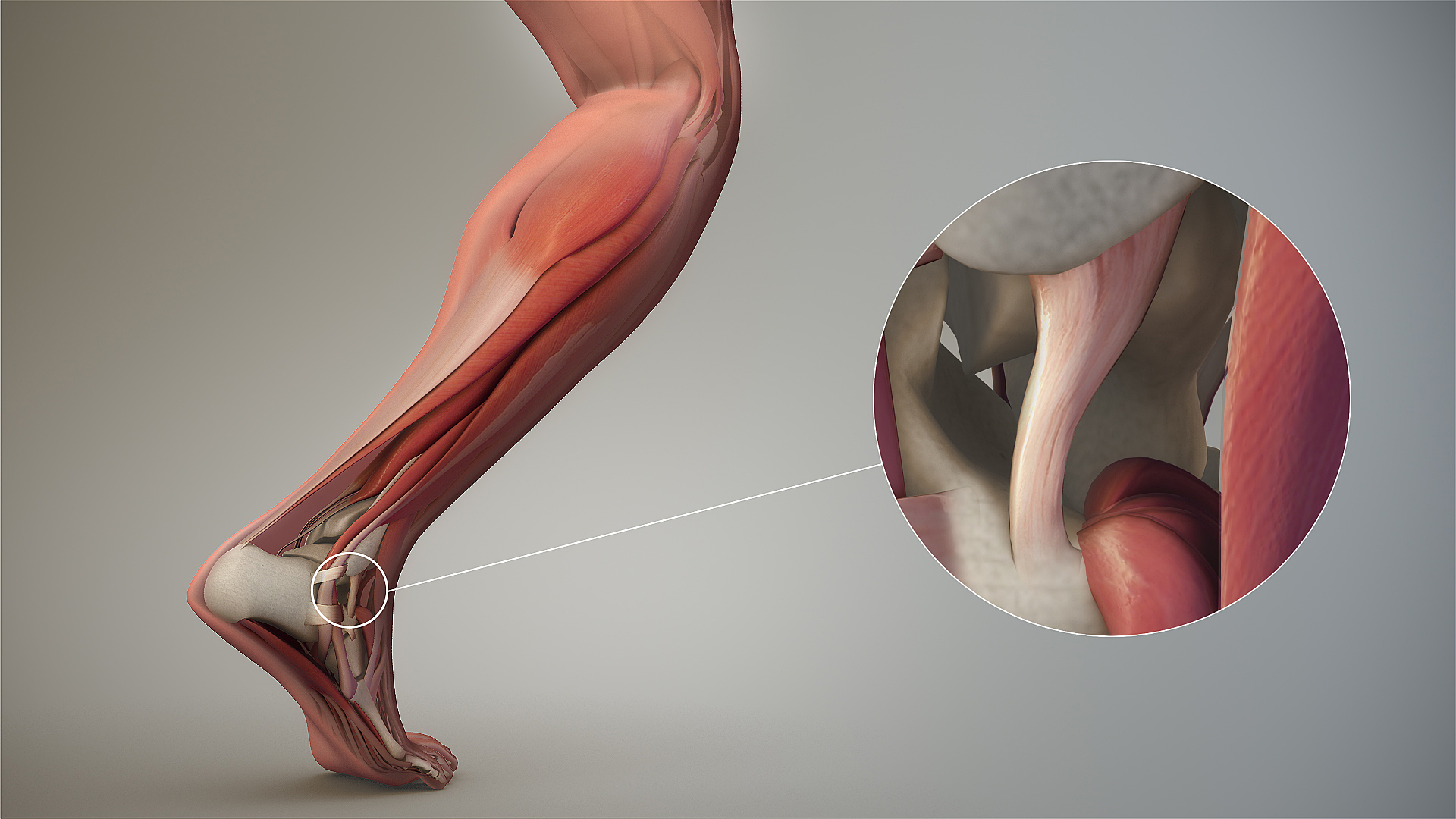
This could happen to you if your ankle dorsiflexors get weak.
/This could happen to you if your ankle dorsiflexors get weak.
This (read below) is actually a normal compensation. Building strength on this compensation without resolving the anterior compartment weakness can lead to knee pain (or other things). It is why, again, we say that asymmetry and especially asymmetrical compensations, can matter in your client.
"muscle strength asymmetry in the ankle joint may lead to counterbalancing muscle strengthening of the knee joint to maintain the center of body mass."
"It is not only the balance between the agonist and antagonist muscles, but also the balance between the left and the right, and between the proximal joint and distal joint in a weight-bearing position that are involved during exercise. As seen in the university players in this study, the weakening of dorsiflexors due to muscle strength asymmetry in the right ankle joint is thought to cause the strengthening of the extension muscles of the knee joint in order to maintain the center of body movement and stability." - Kyoungkyu et al.
What The Gait Guys have to say about this:
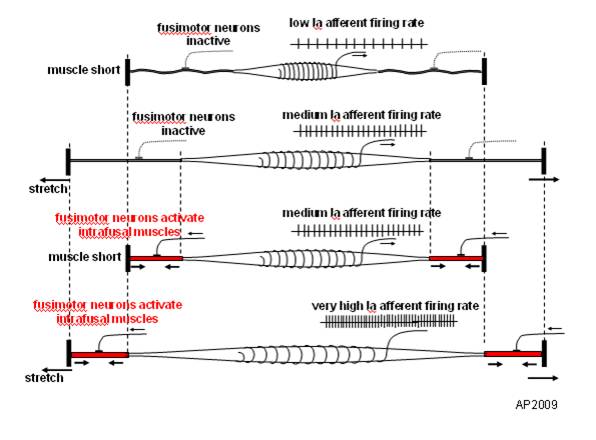
As that foot is approaching the ground, and begins loading, the anterior compartment may not skillfully allow a forefoot loading response and may not protect that anterior ankle mortise joint let alone appropriate and skillful pronation. Ankle dorsiflexion loading may occur too fast and uncontrolled leading to sudden undesirable knee flexion (too much, too fast, too long). After all, closed chain ankle dorsiflexion and knee flexion are deeply paired loading movements. One way to slow down this increased amount of forward tibial progression (ankle dorsiflexion and knee flexion), is to increase the activity of the quadriceps/knee extensors. The compensation of increased knee extension loading will offset the increased knee flexion resulting in improved control the ankle dorisflexion. It is a reasonable compensation, but not one you want to stick around for long or unaddressed. If subtle, and left over time, perhaps even when subclinically presenting, knee pain from increased shear/compression or other mechanical results, may be the first presentation when the true problem is down in the lower region.
Remember, this is about controlling gait and thus center of body mass. This is about not falling over. This is about the central nervous system making necessary adaptations to protect the entire organism, which sometimes means doing anything so as not to fall. Now, just to make this more complicated and fun, imagine that this is a fairly common problem and compensation ON ONE SIDE of the body. So now imagine, the changes in arm swings, maladaptive loading onto the other side, pelvis asymmetry and the list goes on.
Of course, one could just globally add strength to this client, such as more squats, lunges or more deadlifts (instead of a focal intervention at the anterior ankle structures) thus adding another layer of compensation, and perhaps making them feel better, for the time being. Essentially, adding global strength to asymmetry. But make no mistake, this problem is likely to sit here and percolate under the surface with more possible compensations, subtle movement alterations and adaptations, until someone addresses the problem. And remember this, if one does those things long enough, those become a client's new adaptive neuroplastic patterns. Strength first is not always a good first intervention.
J Phys Ther Sci. 2016 Apr; 28(4): 1289–1293.
Effects of muscle strength asymmetry between left and right on isokinetic strength of the knee and ankle joints depending on athletic performance level
Kyoungkyu Jeon, PhD,1 Sungyung Chun, PhD,2,* and Byoungdo Seo, MS, PT3
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4868229/
photo credit: free photos courtesy of Pixabay