We have talked many times here on TGG about pronation, supination, overpronation, asymmetrical pronation, and more.
When most people think of pronation, they think of midfoot pronation, or pronation about the subtalar or transverse tarsal joints. Pronation can actually occur about any articulation or bone, but with respect to the foot, we like to think of rearfoot (ie. talo-calcaneal), midfoot (talo-navicular) and forefoot (transverse tarsal). The question is why does this matter?
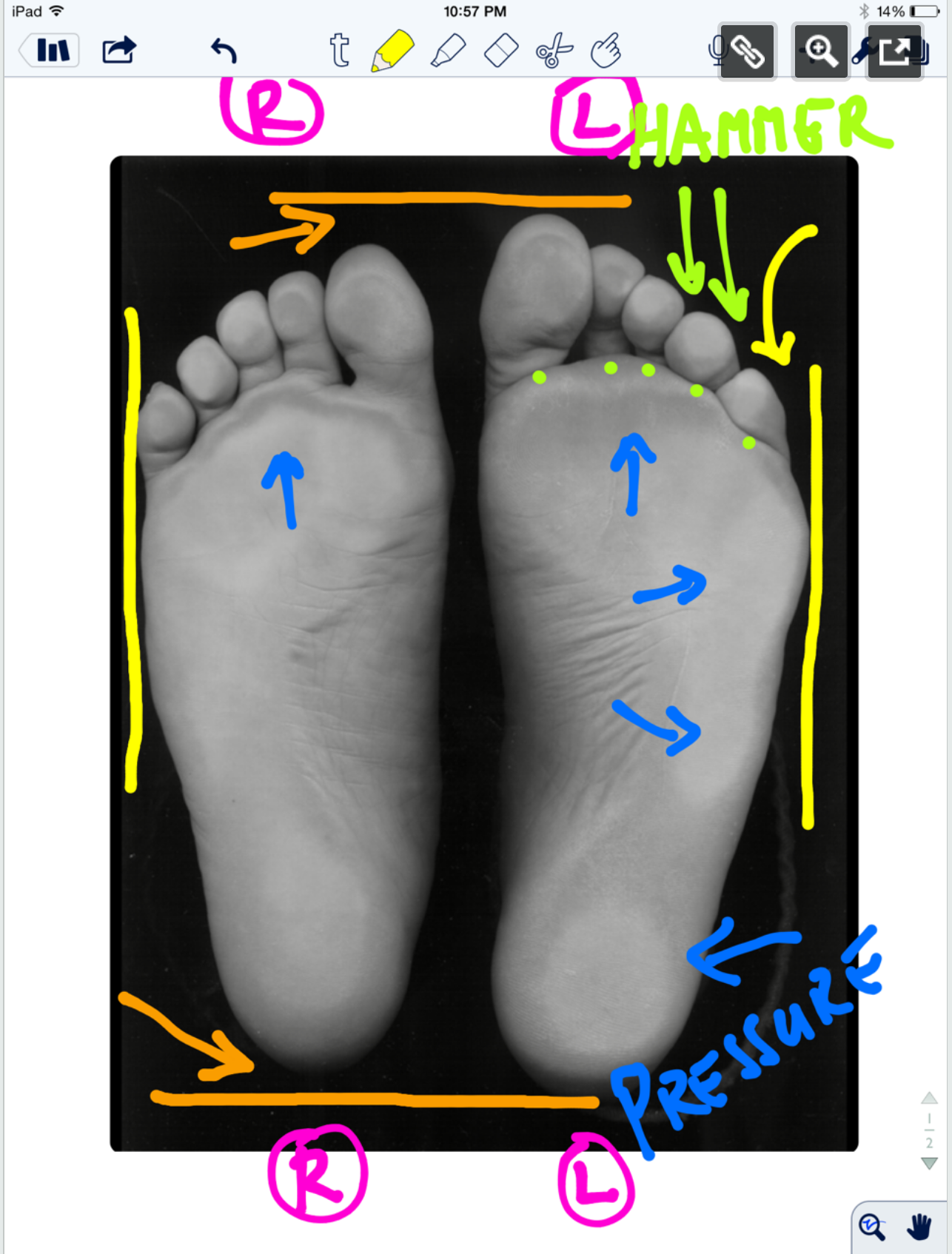
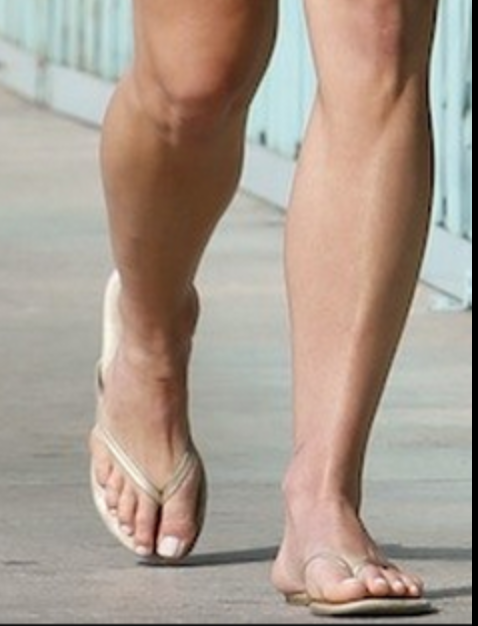
Pronation, with respect to the foot, is defined as a combination of eversion, abduction and dorsiflexion (see picture attached) which results in flattening of the planter vault encompassing the medial and lateral longitudinal arches. In a normal gait cycle, this begins at initial contact (heel strike) and terminates at midstance, lasting no more than 25% of the gait cycle.
In a perfect biomechanical world, shortly following initial contact with the ground, the calcaneus should evert 4-8 degrees, largely because the body of the calcaneus is lateral to the longitudinal axis of the tibia. This results in plantar flexion, adduction and eversion of the talus on the calcaneus, as it slides anteriorly. At this point, there should be dorsiflexion of the transverse tarsal (calcaneo-cuboid and talo-navicular joints). Due to the tight fit of the ankle mortise and its unique shape, the tibial rotates internally (medially). This translates up the kinetic chain and causes internal rotation of the femur, which causes subsequent nutation of the pelvis and extension of the lumbar spine. This should occur in the lower kinetic chain through the 1st half of stance phase. The sequence should reverse after the midpoint of midstance, causing supination and creating a rigid lever for forward propulsion.
Pronation, along with knee and hip flexion, allow for shock absorption during throughout the 1st half of stance phase. Pronation allows for the calcaneo-cuboid and talo-navicular joint axes to be parallel making the foot into a mobile adaptor so it can contour to irregular surfaces, like our hunter gatherer forefathers used to walk on before we paved the planet. Problems arise when the foot either under pronates (7 degrees valgus results in internal tibial rotation), resulting in poor shock absorption or over pronates (> 8 degrees or remains in pronation for greater than 50% of stance phase).
This paper talks about how foot and ankle pathologies have effects on other articulations in the foot. They looked at stance phase of gait in 14 people without pathology at 3 different walking speeds. they found:
coupling relationships between rear foot inversion and hallux plantar flexion and rear foot eversion with hallux dorsiflexion.... When the rear foot everts (as it does as discussed above) during pronation from initial contact to mid stance , the hallux should be extending AND when the rear foot everts, as it should from mid stance to terminal stance/pre swing, the hallux should be plantar flexing to get the 1st ray down to the ground
medial (internal) rotation of there leg was accompanied by mid foot collapse (read pronation) and lateral (external) rotation with mid foot elevation (read supination).... Because of the shape of the talar dome and shape of the talo calcaneal facet joints, the talus plantar flexes, everts and adducts from initial contact to mid stance, and dorsiflexes, inverts and adducts from mid stance to terminal stance/ pre swing
walking speed significantly influenced these coupling relationships....meaning that the faster we go, the faster these things must happen and the greater degree that the surrounding musculature and associated cortical control mechanisms must act
So, when these relationships are compromised, problems (or more often, compensations) ensue. Think about these relationships and the kinetics and kinematics the next time you are studying someones gait.
Dr Ivo Waerlop, one of The Gait Guys
Dubbeldam R1, Nester C, Nene AV, Hermens HJ, Buurke JH. Kinematic coupling relationships exist between non-adjacent segments of the foot and ankle of healthy subjects.Kinematic coupling relationships exist between non-adjacent segments of the foot and ankle of healthy subjects.Gait Posture. 2013 Feb;37(2):159-64. doi: 10.1016/j.gaitpost.2012.06.033. Epub 2012 Aug 27
cool video on our blog to go with this post:
https://www.thegaitguys.com/thedailyblog/2018/8/7/what-do-you-know-about-pronation-and-supination
#gaitanalysis #thegaitguys #pronation #couplingrelationshipsandgait #pronation